Mental health challenges affect 1 in 5 adults annually, with community-level factors playing a significant role in individual wellbeing outcomes.
The Community Mental Wellness and Resilience Act of 2023 highlights the growing recognition that sustainable mental health requires both individual support and community-wide approaches.
We at Devine Interventions understand that building resilient communities starts with accessible resources and meaningful connections that support long-term recovery.
What Makes Community Mental Health Different
Community mental health extends far beyond individual therapy sessions or medication management. Research shows that social isolation and loneliness have a serious impact on physical and mental health, quality of life, and longevity. This dramatic difference stems from shared resources, collective problem-solving, and the safety net that emerges when neighbors actively support each other’s wellbeing.
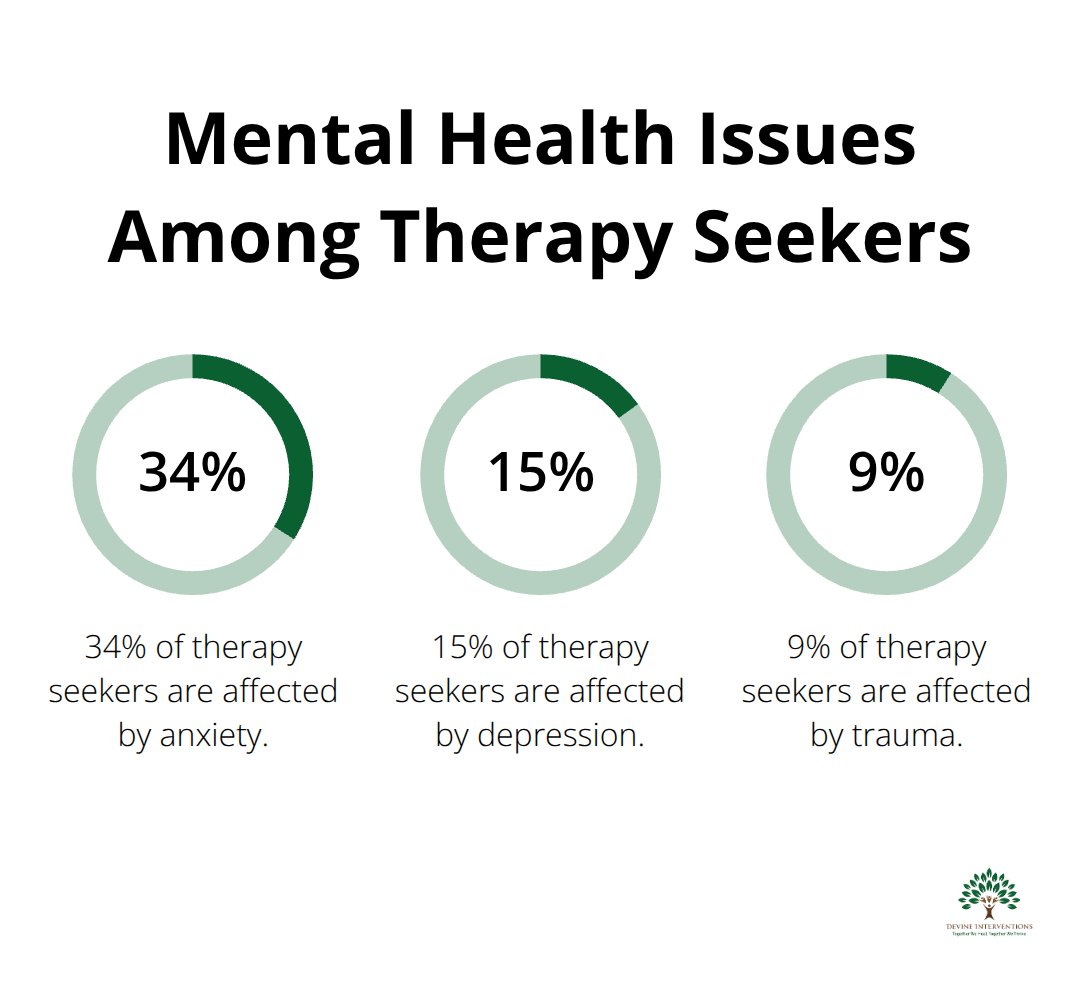
The Statistics Paint a Clear Picture
Recent data from the National Alliance on Mental Illness reveals that 83% of therapists observed increased first-time therapy seekers in 2023, with Millennials representing 53% of current clients. Anxiety affects 34% of those who seek help, followed by depression at 15% and trauma at 9%. These statistics reflect a broader community crisis where individual struggles compound into neighborhood-wide challenges.
Areas with limited mental health resources see suicide rates 40% higher than communities with integrated support systems.
Individual Recovery Needs Community Foundation
The connection between personal and community wellbeing operates as a reinforcement cycle. When one person receives effective mental health treatment, their improved function strengthens family relationships, workplace productivity, and social connections. The REACH NOLA initiative demonstrated this principle after Hurricane Katrina, where it trained over 400 community providers and created measurable improvements in neighborhood mental health outcomes.
How Social Networks Shape Mental Health
Strong communities produce resilient individuals through volunteer work, mentorship, and economic contribution. Research from the National Institute of Standards and Technology (NIST) emphasizes that interdependencies among community resources create more effective recovery outcomes. Communities that prioritize social connectedness through events and activities exhibit greater adaptability during crises.
Professional Services Bridge Individual and Community Needs
While community support provides the foundation, professional mental health services offer specialized interventions that strengthen both individuals and their networks. This combination creates the most effective approach to mental wellness, where clinical expertise meets community connection to address complex mental health challenges that require both professional guidance and peer support.
How Communities Build Mental Health Resilience
Community mental health programs succeed when they prioritize peer support networks and grassroots leadership over top-down approaches. Communities that integrate mental health services into crisis response strategies achieve better recovery outcomes during successive climate events and emergencies. Programs like community health worker training create sustainable change because local residents understand cultural nuances and build trust faster than outside professionals.
Evidence-Based Community Strategies
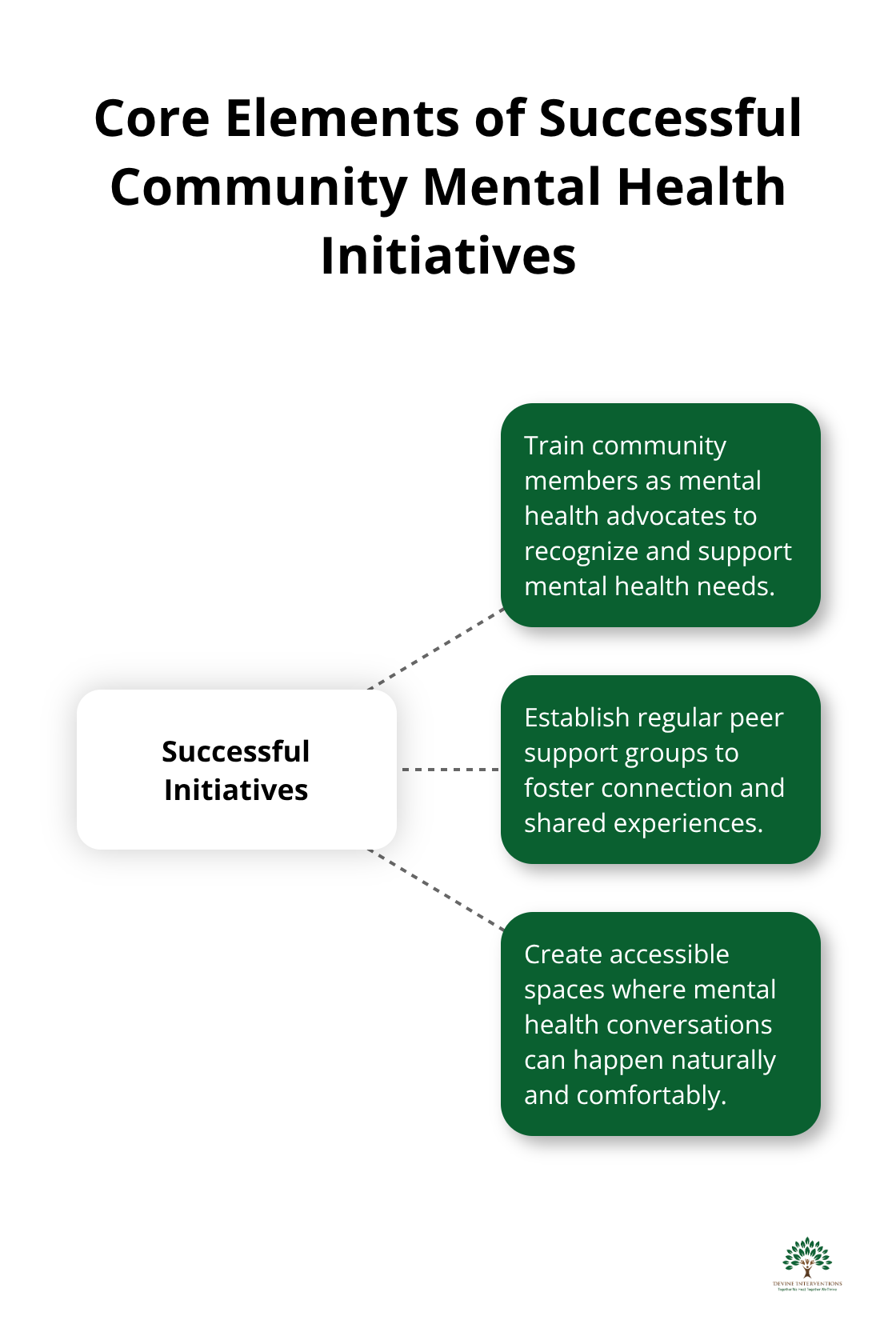
Successful initiatives focus on three core elements: they train community members as mental health advocates, establish regular peer support groups, and create accessible spaces where conversations happen naturally. Communities with high social capital enjoy better mental health outcomes and demonstrate greater capability for resilience during crises. These programs work because they address the treatment gap that exceeds 85% in many underserved areas.
Peer Networks Drive Real Change
Social connections function as the strongest predictor of mental health recovery, with isolated individuals facing higher rates of depression and anxiety. Research shows that bisexual adults experience stress and depression at rates of 34.3%–54.4%. Communities that organize monthly mental health check-ins, neighborhood support groups, and skill-sharing workshops see measurable improvements in collective wellbeing. The key lies in consistency rather than intensity – weekly 90-minute peer support meetings produce better outcomes than monthly all-day events.
Participants develop coping strategies through shared experiences and create informal support systems that operate beyond scheduled programming. These networks provide validation and foster belonging during difficult times, which research shows significantly reduces feelings of isolation after adverse events.
Safe Conversation Spaces Need Structure
Mental health conversations require intentional design to move beyond surface-level check-ins toward meaningful support. Effective community spaces establish clear communication guidelines, trained facilitators, and confidentiality agreements that protect vulnerable sharing. Libraries, community centers, and faith-based organizations that dedicate specific times for mental health discussions report higher engagement than informal approaches.
These structured conversations reduce stigma by normalizing mental health challenges as common human experiences rather than personal failures. They encourage more residents to seek professional help when community support reaches its limits, which creates the perfect bridge to understanding when professional intervention becomes necessary.
When Professional Help Becomes Necessary
Community support reaches its limits when symptoms persist despite peer networks, interfere with daily function, or involve thoughts of self-harm. Professional intervention becomes time-sensitive rather than optional for severe mental health challenges. Inadequate access to behavioral health services disproportionately impacts marginalized populations who live in disadvantaged areas.
Warning Signs That Require Professional Care
Warning signs that community support alone won’t suffice include persistent sleep disruption that lasts more than two weeks, inability to maintain work or school responsibilities, substance use as a coping mechanism, or panic attacks that limit normal activities. When someone experiences thoughts of self-harm, professional intervention becomes immediately necessary regardless of community support availability. Chronic symptoms that don’t respond to peer support after 4-6 weeks typically require clinical assessment and specialized treatment approaches.
Professional Services Bridge Critical Gaps
Mental health professionals offer specialized interventions that community peers cannot provide, including psychiatric medication management, trauma-focused therapy techniques, and crisis intervention protocols. Individual therapy sessions average 45-50 minutes and utilize evidence-based approaches like Cognitive Behavioral Therapy and trauma-informed care that require professional training to implement safely. Group therapy combines professional facilitation with peer support, which creates structured environments where participants learn coping strategies under clinical supervision.
Intensive Outpatient Programs provide 9-12 hours of weekly treatment while they allow clients to maintain daily responsibilities. This fills the gap between community support and full hospitalization. Partial Hospitalization Programs offer structured daily treatment for those who require more intensive care than traditional outpatient services.
Access Barriers Require Strategic Solutions
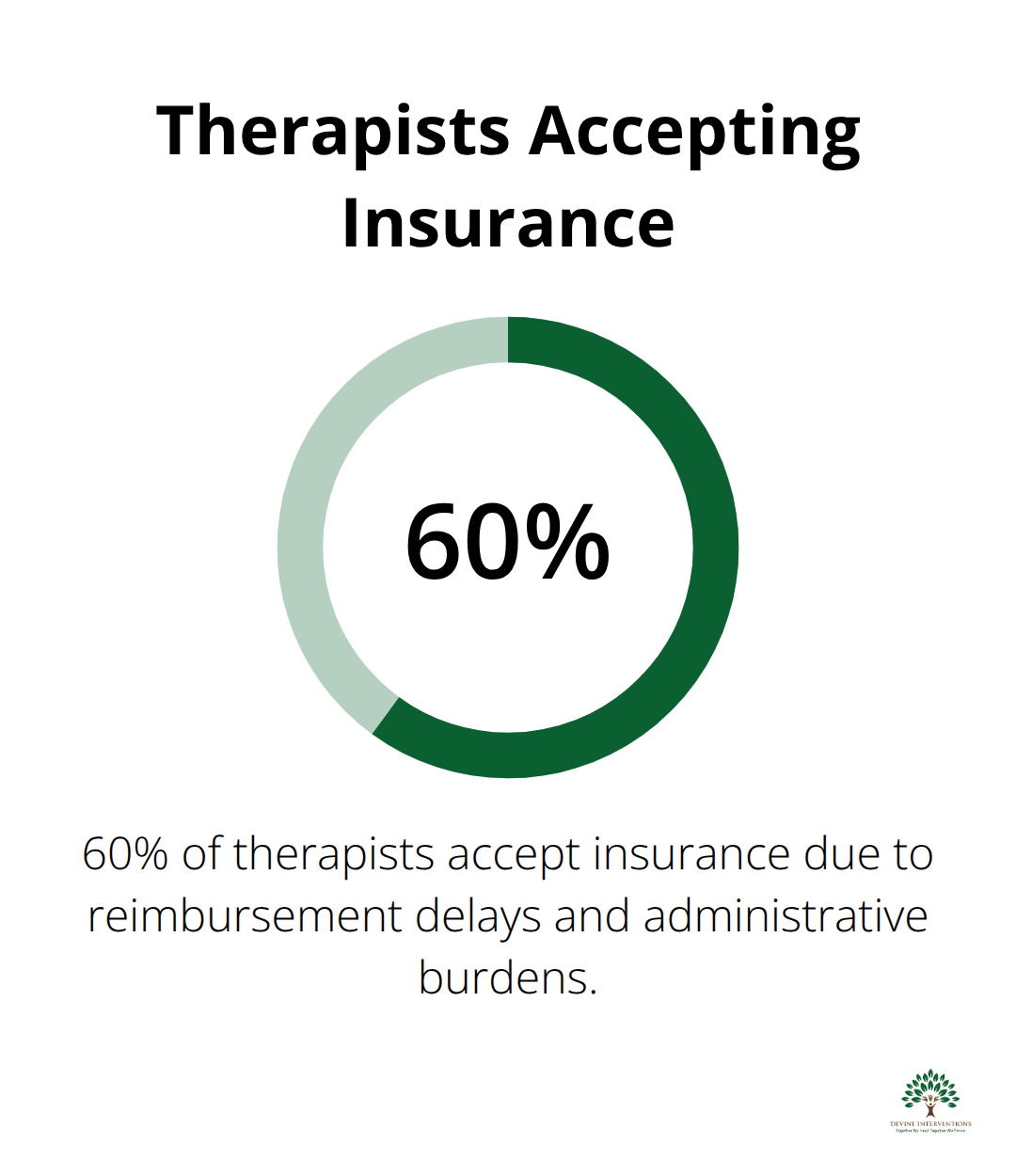
Insurance coverage remains the primary obstacle, with only 60% of therapists who accept insurance due to reimbursement delays and administrative burdens. Many practices now provide detailed superbills for out-of-network reimbursement, which allows clients to recover portions of their investment through insurance benefits (typically 50-80% depending on plan specifics). Payment plans and fee scales make professional care accessible regardless of immediate financial capacity.
Telehealth options eliminate transportation barriers and schedule conflicts that prevent consistent treatment engagement. Professional practices that offer flexible payment options, transparent fee structures, and comprehensive stress management help navigate insurance complexities while they maintain focus on clinical outcomes rather than administrative obstacles.
Final Thoughts
The Community Mental Wellness and Resilience Act of 2023 recognizes what research has consistently shown: sustainable mental health requires both community connection and professional expertise that work in harmony. Neither approach alone produces the comprehensive support that individuals need for lasting recovery. Communities provide the foundation through peer networks, shared experiences, and daily encouragement that professional services cannot replicate, while professional care offers specialized interventions and evidence-based treatments that community support cannot provide.
Community mental health transformation starts with small, consistent actions that residents can implement immediately. Organize monthly mental health check-ins in your neighborhood where people can share experiences safely. Train community members as mental health advocates who can recognize when professional intervention becomes necessary (this creates the bridge between peer support and clinical care).
We at Devine Interventions bridge this gap through comprehensive mental health services that combine clinical excellence with community integration. Our approach supports both immediate crisis intervention and long-term recovery goals. Professional services provide the specialized tools that transform community support into sustainable wellness, creating pathways where clinical expertise meets peer connection for lasting mental health outcomes.