Schools across America face a mental health crisis, with 1 in 5 students experiencing significant emotional challenges. The Improving Mental Health and Wellness in Schools Act offers new hope and resources.
We at Devine Interventions understand how overwhelming implementation can feel. This comprehensive guide breaks down the Act’s requirements and provides practical strategies for creating effective mental health programs in your school community.
What Does the New Mental Health Act Actually Require?
The Bipartisan Safer Communities Act of 2022 allocated federal mental health grants for youth mental health initiatives in schools. However, the Education Department has recently cut approximately $1 billion worth of these federal mental health grants that were approved by Congress.
Schools must establish comprehensive mental health programs that include universal screenings, early intervention services, and crisis response protocols. The Act requires districts to create Multi-Tiered Systems of Support with different levels of care intensity. Staff members must complete mental health awareness programs within 18 months of implementation.
Federal Funding Streams and State Requirements
States can now access Medicaid reimbursements for school-based mental health services through new Centers for Medicare & Medicaid Services provisions. Illinois leads with mandatory annual mental health screenings that start in 2027-28 for grades three through twelve (providing screening materials at no cost to districts).
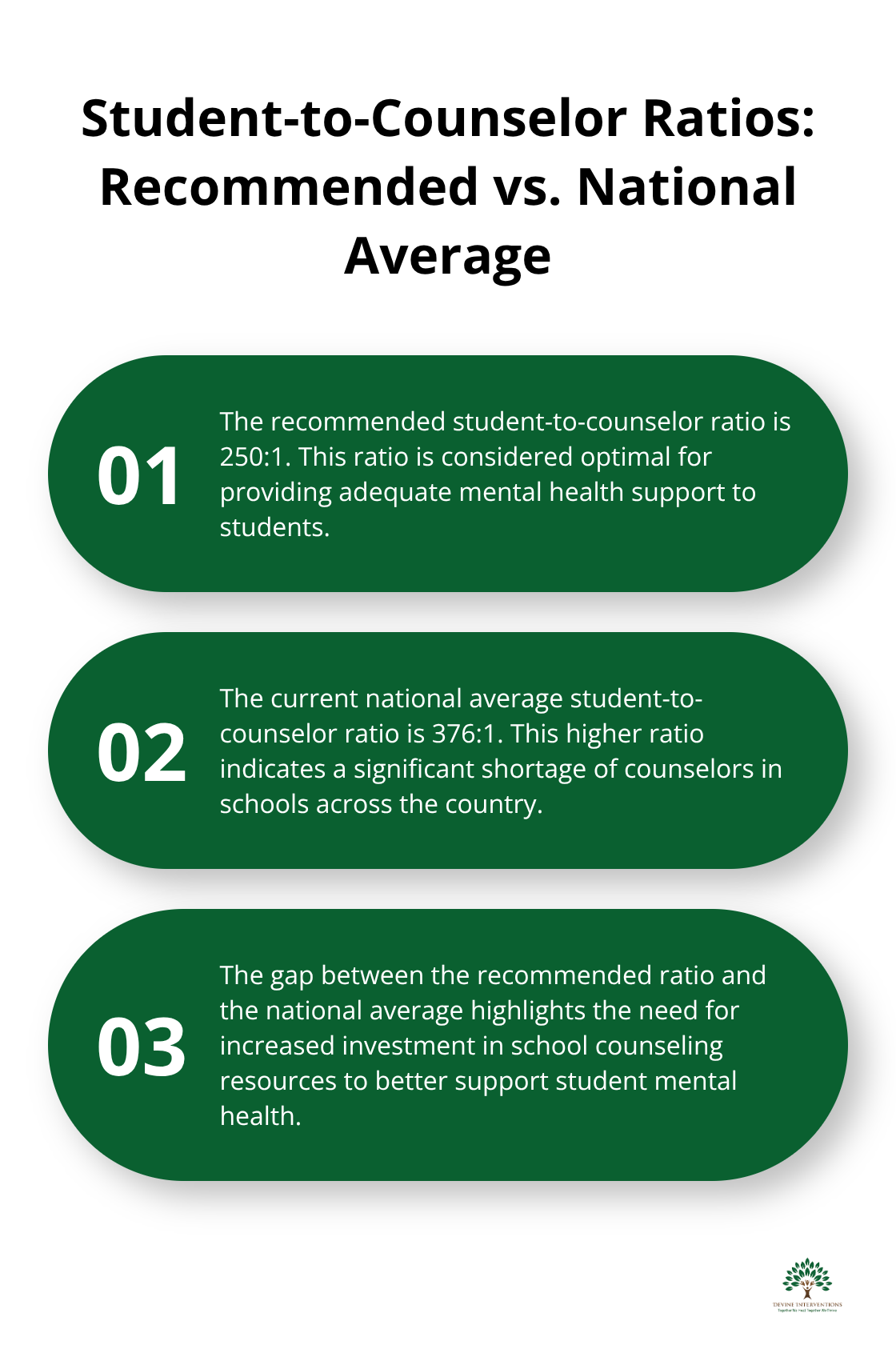
The recommended student-to-counselor ratio stands at 250:1, though the national average currently reaches 376:1. Schools must hire additional mental health professionals or partner with community providers to meet federal guidelines. Districts that receive federal funds must demonstrate measurable outcomes through data collection and reporting systems.
Implementation Deadlines and Compliance Standards
The Act requires schools to establish mental health programs by September 2025, with full compliance expected by 2027. Districts must submit annual progress reports that document student outcomes, staff completion rates, and service utilization statistics.
Schools that fail to meet implementation deadlines risk losing federal funding eligibility. The legislation emphasizes evidence-based practices and requires programs to demonstrate effectiveness through peer-reviewed research. Community partnerships become essential, as schools must coordinate with local mental health providers to expand service capacity beyond traditional school hours.
These requirements create new opportunities for schools to partner with established mental health providers who understand both clinical excellence and practical implementation challenges.
What Mental Health Strategies Actually Work in Schools
Schools need concrete strategies that produce measurable results, not theoretical frameworks. The Good Behavior Game creates supportive classroom environments while reducing disruptions by 23% according to American Psychological Association research. Universal screening identifies at-risk students before crises develop, with schools implementing these evidence-based approaches seeing significant improvements in both academic performance and behavioral outcomes.
Early Detection Through Systematic Screening
Illinois leads the nation with mandatory annual mental health screenings starting in 2027-28 for grades three through twelve, providing materials at no cost to districts. Students who receive mental health services in school settings are six times more likely to complete treatment compared to community-based services (according to New Orleans research data). Universal screening tools like the Strengths and Difficulties Questionnaire detect anxiety, depression, and behavioral concerns within 15 minutes per student.
Schools that use systematic screening report 30% fewer disciplinary incidents and improved attendance rates. The key lies in connecting screening results to immediate intervention services rather than letting identified students wait months for appointments.
Professional Development That Creates Real Change
Mental Health First Aid training for teachers improves their knowledge, skills, attitudes, and self-efficacy in supporting students. Teachers who complete trauma-informed practice training create environments where students with mental health challenges show 25% better academic performance. The most effective programs require all staff members to complete 8-hour initial training followed by quarterly refresher sessions.
Schools that implement comprehensive staff training report decreased teacher turnover and improved job satisfaction. Training must focus on practical skills like crisis de-escalation and connecting students to resources, not just awareness sessions that produce minimal behavioral change.
Student-Led Support Networks
Peer support programs create resilience among students while reducing the stigma around mental health help-seeking. Students who participate in peer support initiatives show 40% better emotional regulation and increased willingness to seek professional help when needed. These programs work best when schools train student leaders in basic mental health awareness and provide structured supervision from qualified staff members.
However, even the best school-based programs sometimes need additional support from specialized mental health providers who understand both clinical excellence and practical implementation challenges.
What Stops Schools From Building Mental Health Programs
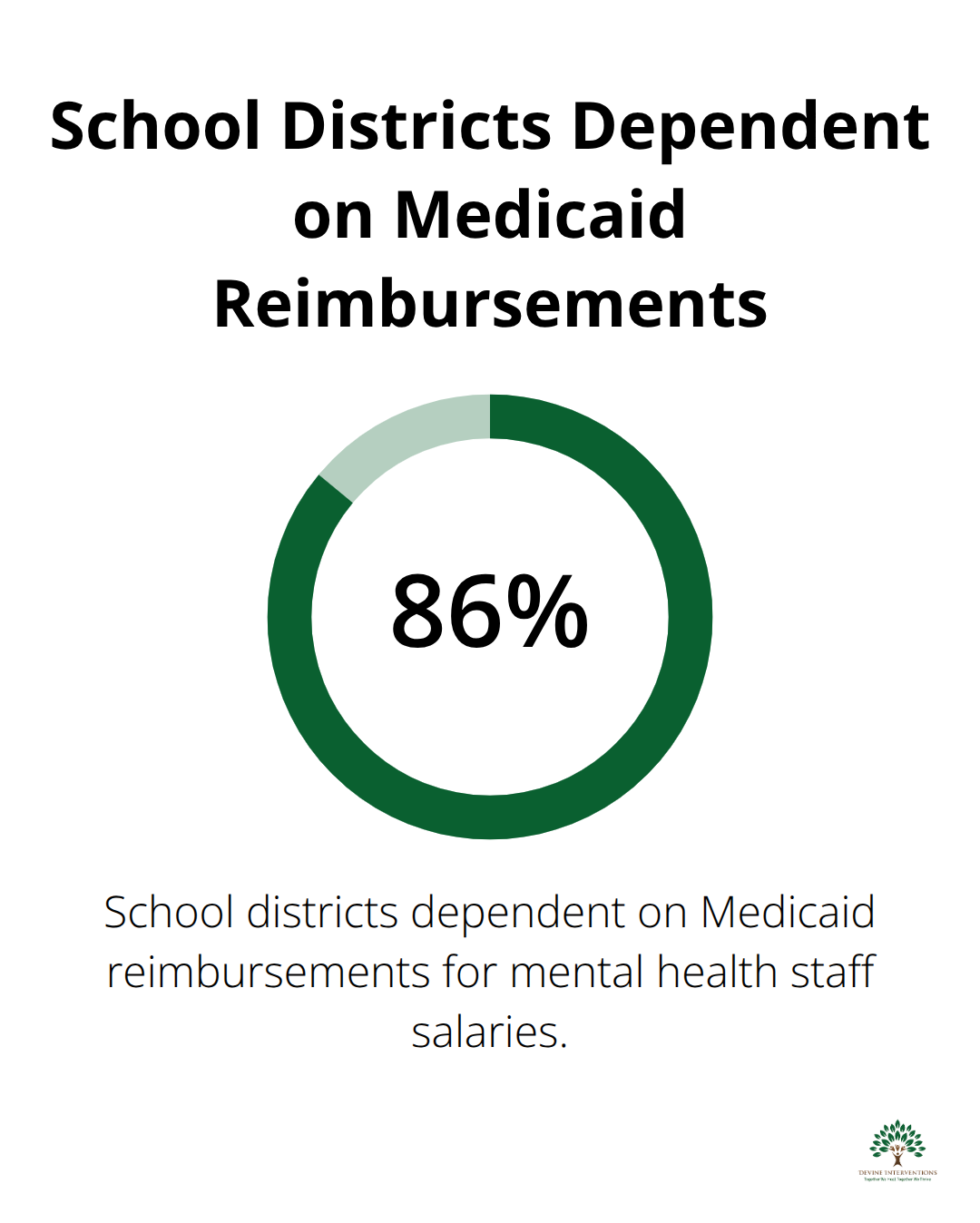
The expiration of Elementary and Secondary School Emergency Relief funding has left 86% of school districts dependent on Medicaid reimbursements for mental health staff salaries according to recent surveys. Schools face an average shortfall of $2.3 million annually when they implement comprehensive mental health programs, with rural districts that experience 40% higher costs due to limited local provider networks. The national shortage of school psychologists creates a 1,065:1 student ratio compared to the recommended 500:1, which forces districts to prioritize crisis response over prevention programs that produce better long-term outcomes.
Budget Shortfalls That Cripple Program Development
Districts lose federal funding when they fail to meet implementation deadlines, yet they lack resources to hire qualified staff. The average school psychologist salary reaches $78,000 annually, while districts need at least three full-time positions to serve 1,500 students effectively. Rural schools pay 25% more for mental health professionals due to limited candidate pools and higher recruitment costs.
States that expanded Medicaid reimbursement for school-based services report 60% better program sustainability. However, administrative costs for Medicaid billing consume 15-20% of reimbursement funds (according to district financial reports). Schools that partner with established mental health providers reduce overhead costs while maintaining service quality.
Staff Resistance That Undermines Implementation
Teachers resist mental health training when they perceive additional responsibilities without adequate compensation or administrative support. Districts that mandate 8-hour Mental Health First Aid training without workload adjustments see 35% higher staff turnover within two years. Successful implementation requires principals to reduce non-essential meetings by 20% and provide substitute coverage during training sessions.
Schools that offer stipends for mental health training completion and create peer mentorship programs report 60% better staff buy-in and program sustainability. The most effective approach involves training volunteer teacher leaders first, then uses their success stories to motivate broader staff participation rather than mandate universal training immediately.
Measurement Systems That Miss the Mark
Schools struggle to measure mental health program effectiveness because they focus on clinical metrics instead of educational outcomes that administrators value. Tracking suspension rates, chronic absenteeism, and academic performance provides concrete evidence of program impact that school boards understand. Districts that use Student Risk Screening Scale data report fewer emergency interventions and improved crisis response outcomes.
Administrators need quarterly reviews that connect mental health services directly to improved graduation rates and reduced disciplinary incidents. Schools that establish baseline measurements before program launch demonstrate clear return on investment through data-driven reporting systems that include stress management and anxiety management components.
Final Thoughts
The Improving Mental Health and Wellness in Schools Act creates unprecedented opportunities for student wellbeing through systematic screening, evidence-based interventions, and sustainable funding mechanisms. Schools that implement comprehensive programs see 30% fewer disciplinary incidents, improved attendance rates, and better academic outcomes for all students. Districts must act now to secure federal funding before September 2025 deadlines.
Schools should start with universal screening programs, train staff in Mental Health First Aid, and establish community partnerships with qualified providers. Districts that partner with established mental health organizations reduce implementation costs while they maintain clinical excellence. The long-term impact extends beyond individual students to entire communities (early intervention prevents crises, reduces emergency room visits, and creates supportive environments where all students can thrive academically and emotionally).
We at Devine Interventions understand the challenges schools face when they implement mental health programs. Our team provides comprehensive mental health services that support school initiatives with evidence-based practices and compassionate care. Contact us today to learn how we can support your district’s mental health programs with measurable results.







