Trauma affects millions of people worldwide, leaving lasting impacts on mental health and daily functioning. Recovery requires the right tools and guidance to rebuild your sense of safety and well-being.
We at Devine Interventions understand that healing from trauma takes time, patience, and evidence-based approaches. This trauma-focused therapy workbook provides practical strategies and professional insights to support your journey toward recovery and resilience.
What Actually Happens to Your Brain During Trauma
The Physical Reality of Trauma Impact
Trauma fundamentally rewires your brain’s structure and function. The amygdala, your brain’s alarm system, becomes hyperactive after traumatic experiences and triggers fight-or-flight responses even when you’re safe. Emergent evidence suggests that trauma exposure and resultant PTSD symptoms are associated with altered structure and function of the brain’s visual processing areas. This explains why traumatic memories feel fragmented or why you might struggle with concentration and decision-making months or years later.
Your nervous system gets stuck in survival mode. The vagus nerve, which controls your rest-and-digest functions, becomes dysregulated. This creates physical symptoms like rapid heartbeat, shallow breathing, and digestive issues that persist long after the traumatic event ended. The prefrontal cortex, responsible for logical thinking and emotional regulation, goes offline during trauma responses and makes it nearly impossible to think clearly or calm yourself down.
Recognizing Trauma’s Hidden Symptoms
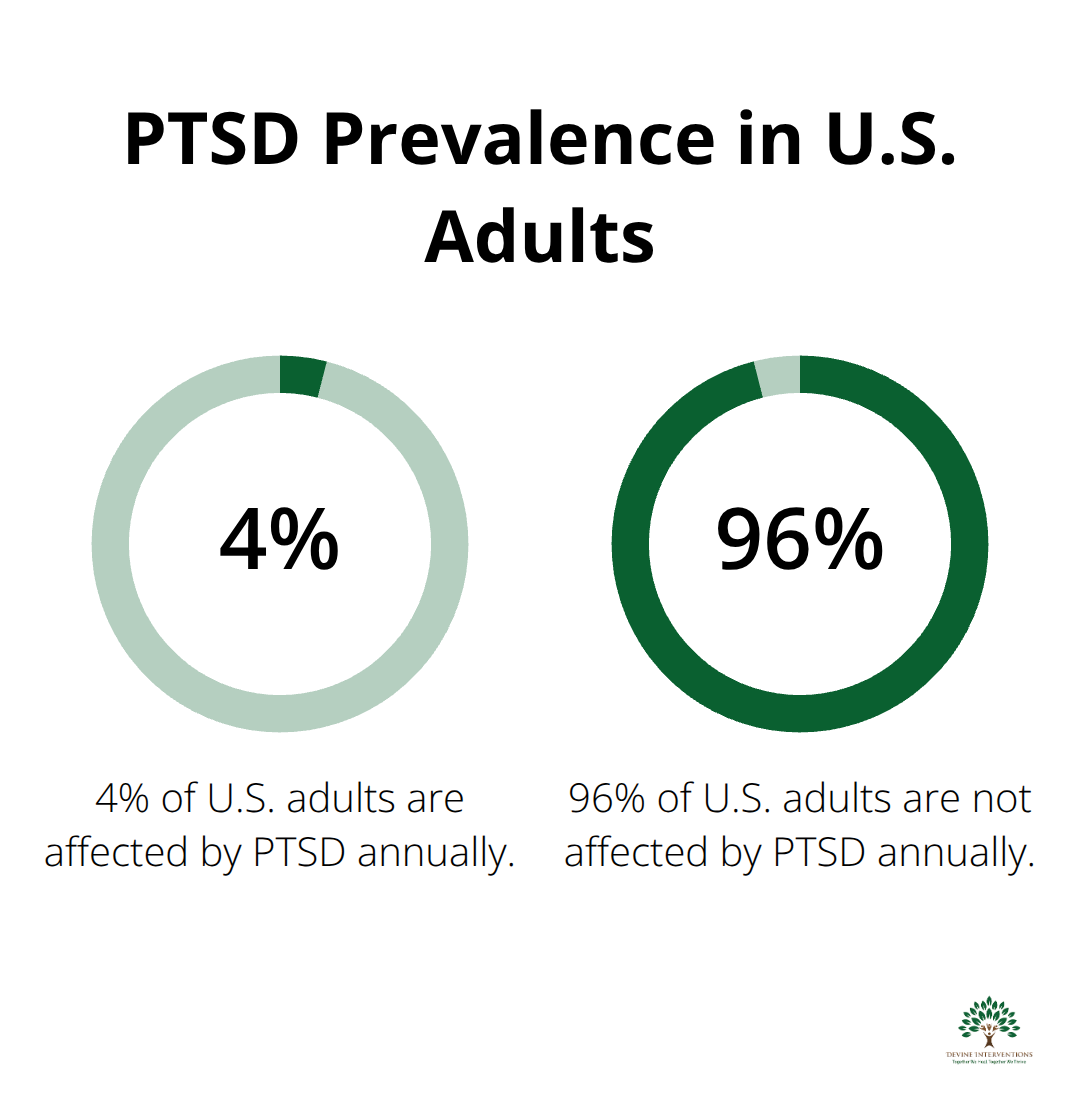
Trauma manifests differently than most people expect. PTSD affects approximately 4% of U.S. adults annually, but many cases go undiagnosed because symptoms don’t match typical expectations. Instead of flashbacks, you might experience emotional numbness, difficulty trusting others, or feel disconnected from your body. Sleep disturbances affect many trauma survivors and create a cycle where exhaustion makes emotional regulation even harder.
Hypervigilance keeps your nervous system scanning for threats constantly. You might startle easily, feel exhausted without clear reason, or struggle with boundaries in relationships. These aren’t character flaws or signs of weakness. Your brain adapted to protect you during dangerous situations, and now it needs specific techniques to learn safety again.
How Trauma Disrupts Daily Life
The brain changes from trauma extend far beyond emotional responses. Your ability to process new information becomes compromised when your nervous system operates in constant alert mode. Simple tasks like grocery shopping or attending meetings can feel overwhelming because your brain interprets normal stimuli as potential threats.
Trauma also affects your relationship with time and memory. You might lose hours to dissociation or feel like traumatic events happened yesterday even when they occurred years ago. These disruptions make it difficult to plan for the future or feel grounded in the present moment.
Understanding these neurological changes helps explain why willpower alone isn’t enough to overcome trauma’s effects. Your brain needs targeted therapeutic approaches to restore healthy functioning and create new neural pathways that support healing.
Evidence-Based Trauma Therapy Approaches
Cognitive Behavioral Therapy Rewires Trauma Responses
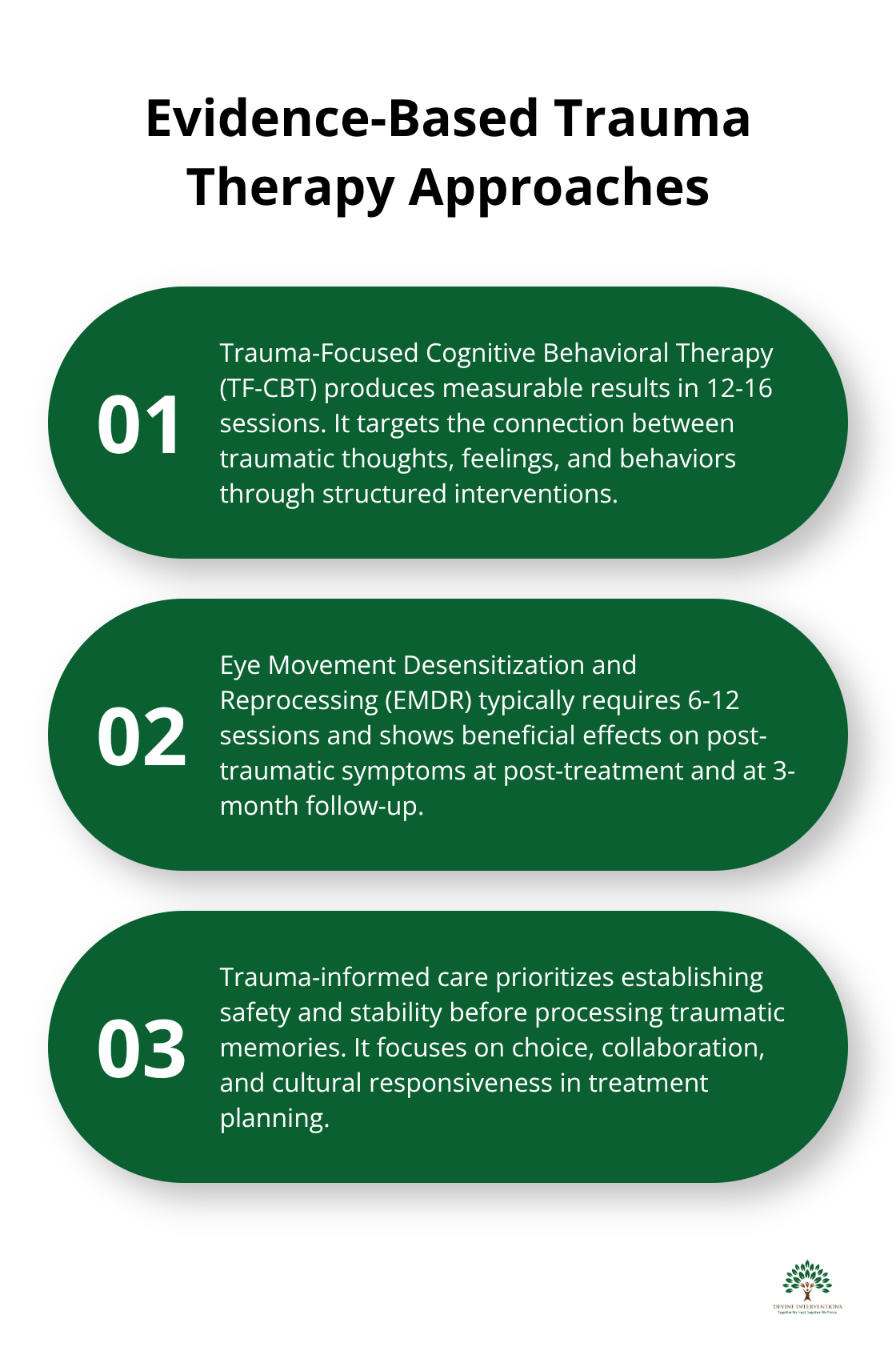
Trauma-Focused Cognitive Behavioral Therapy produces measurable results in 12-16 sessions according to clinical research. This approach targets the connection between traumatic thoughts, feelings, and behaviors through structured interventions. TF-CBT breaks down into specific phases: psychoeducation about trauma responses, relaxation training, cognitive processing of distorted thoughts, and gradual exposure to trauma reminders.
The Feelings Thermometer worksheet helps you rate emotional intensity from 1-10 and gives your therapist concrete data about your progress. Cognitive restructuring tools identify specific thought distortions like catastrophic thinking or all-or-nothing patterns that keep you stuck in trauma responses. These worksheets serve as bridges between sessions and facilitate continued skill application outside the clinical environment.
EMDR and Somatic Approaches Target Body-Stored Trauma
Eye Movement Desensitization and Reprocessing works when it activates your brain’s natural healing processes while you recall traumatic memories. EMDR typically requires 6-12 sessions and shows beneficial effects on post-traumatic symptoms at post-treatment and at 3-month follow-up. During sessions, you track your therapist’s finger movements while processing traumatic memories, which helps your brain reintegrate fragmented trauma memories.
Somatic therapies like the NeuroAffective Relational Model work with the effects of complex and developmental trauma. These body-based approaches recognize that trauma lives in your nervous system (not just your thoughts) and require embodied processes for complete resolution.
Trauma-Informed Care Creates Safety First
Effective trauma treatment starts with establishing safety and stability before processing traumatic memories. The 5-4-3-2-1 grounding technique helps regulate your nervous system when it engages all five senses: identify 5 things you see, 4 you can touch, 3 you hear, 2 you smell, and 1 you taste. This technique provides immediate relief during overwhelming moments.
Trauma-informed practitioners understand that traditional therapy approaches can retraumatize clients, so they prioritize choice, collaboration, and cultural responsiveness in treatment planning. They create environments where you maintain control over your healing process and move at your own pace. These foundational safety principles prepare you to build your own personalized toolkit of healing strategies.
How Do You Build Practical Tools for Daily Healing
Immediate Response Techniques That Actually Work
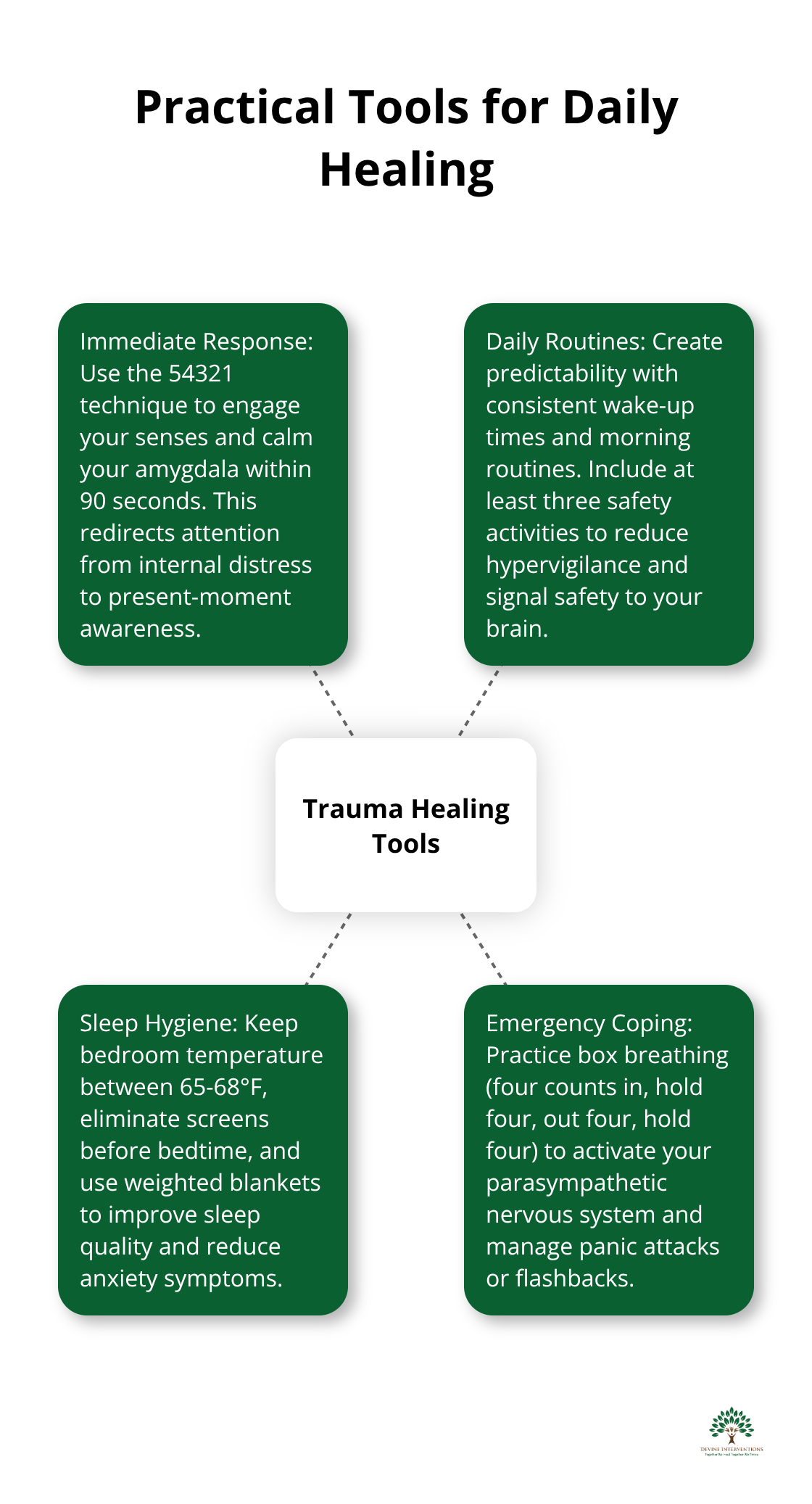
Your nervous system needs specific interventions when trauma responses activate unexpectedly. The 54321 technique works because it redirects your attention from internal distress to present-moment awareness through your senses. Research shows that art therapy combined with mindfulness yields significant decreases in measures of anxiety, depression, and shame. Start with five things you can see around you, then four things you can physically touch, three sounds you hear, two scents you notice, and one taste in your mouth. This sequence engages your prefrontal cortex and calms your amygdala within 90 seconds.
Progressive muscle relaxation provides another immediate tool for trauma responses. Tense each muscle group for five seconds, then release completely. Start with your toes and work up to your face. This technique teaches your body the difference between tension and relaxation (which many trauma survivors have forgotten). Cold water on your wrists or face activates your vagus nerve and triggers your body’s natural calm response. Keep ice cubes in your freezer specifically for trauma responses.
Daily Routines That Create Stability
Daily routines create predictability that your traumatized nervous system desperately needs. Wake up at the same time every day and create a morning routine that includes at least three safety activities. This might include door lock checks, daily schedule reviews, or ten-minute breath exercises. Consistency signals safety to your brain and reduces the hypervigilance that exhausts trauma survivors.
Sleep hygiene becomes non-negotiable for trauma recovery. Keep your bedroom temperature between 65-68 degrees Fahrenheit and eliminate all screens two hours before bedtime. Create a bedtime ritual that includes three positive daily experiences written down. This practice rewires your brain to notice positive experiences instead of constant threat scanning. Weighted blankets improve symptoms of insomnia and total sleep time, and significantly improve symptoms of anxiety in psychiatric patients.
Your Personal Safety Network
Trauma recovery requires human connection, but many survivors struggle with trust and boundaries. Start with one person who feels genuinely safe and practice small, non-traumatic information shares with them. This builds your capacity for connection without nervous system overwhelm. Schedule regular check-ins with this person (even five-minute phone calls twice per week work well).
Develop specific phrases you can use when you feel unsafe or triggered in social situations. Practice “I need to step outside for a moment” or “I’m going to take a break” until these responses become automatic. Create a safety plan that includes specific people to call, places to go, and activities that calm your nervous system. Write this plan down and keep copies in multiple locations so you can access it when your thinking becomes unclear during trauma responses.
Emergency Coping Strategies
Panic attacks and flashbacks require immediate intervention techniques that work within minutes. Box breathing (four counts in, hold four, out four, hold four) activates your parasympathetic nervous system and stops the escalation of panic symptoms. Practice this technique daily so it becomes automatic during crisis moments.
Temperature changes provide rapid nervous system regulation. Hold ice cubes, splash cold water on your face, or step outside into different air temperature. These techniques activate your dive reflex and immediately slow your heart rate. Keep a small ice pack in your car or workplace for unexpected trauma responses. Physical movement like jumping jacks or wall push-ups can discharge the energy that builds up during fight-or-flight activation.
Final Thoughts
Trauma recovery follows a predictable path when you combine evidence-based techniques with professional support. Your brain’s neuroplasticity means that complete recovery remains possible regardless of how long trauma has affected your life. The techniques and strategies outlined in this trauma-focused therapy workbook provide immediate relief while you build long-term resilience.
Professional support becomes necessary when trauma symptoms interfere with work, relationships, or daily tasks for more than a month. Persistent sleep disturbances, emotional numbness, or hypervigilance that doesn’t respond to self-help techniques require trauma-focused therapy to accelerate your recovery process. These symptoms indicate that your nervous system needs specialized intervention beyond what any workbook can provide.
We at Devine Interventions understand that you need courage to take the first step toward professional help. Recovery isn’t about who you were before trauma occurred but about how you integrate your experiences and build a stronger, more resilient version of yourself. With the right tools and professional guidance, you can reclaim your sense of safety and create meaningful connections again.