Living with a chronic illness brings unique emotional challenges that extend far beyond physical symptoms. The psychological impact often catches people off guard, affecting relationships, daily routines, and overall mental well-being.
We at Devine Interventions understand that developing effective coping strategies for chronic illness requires both practical tools and emotional support. This guide offers evidence-based approaches to help you navigate the complex journey of managing your mental health alongside your physical condition.
Understanding the Emotional Impact of Chronic Illness
The Shock of Redefinition
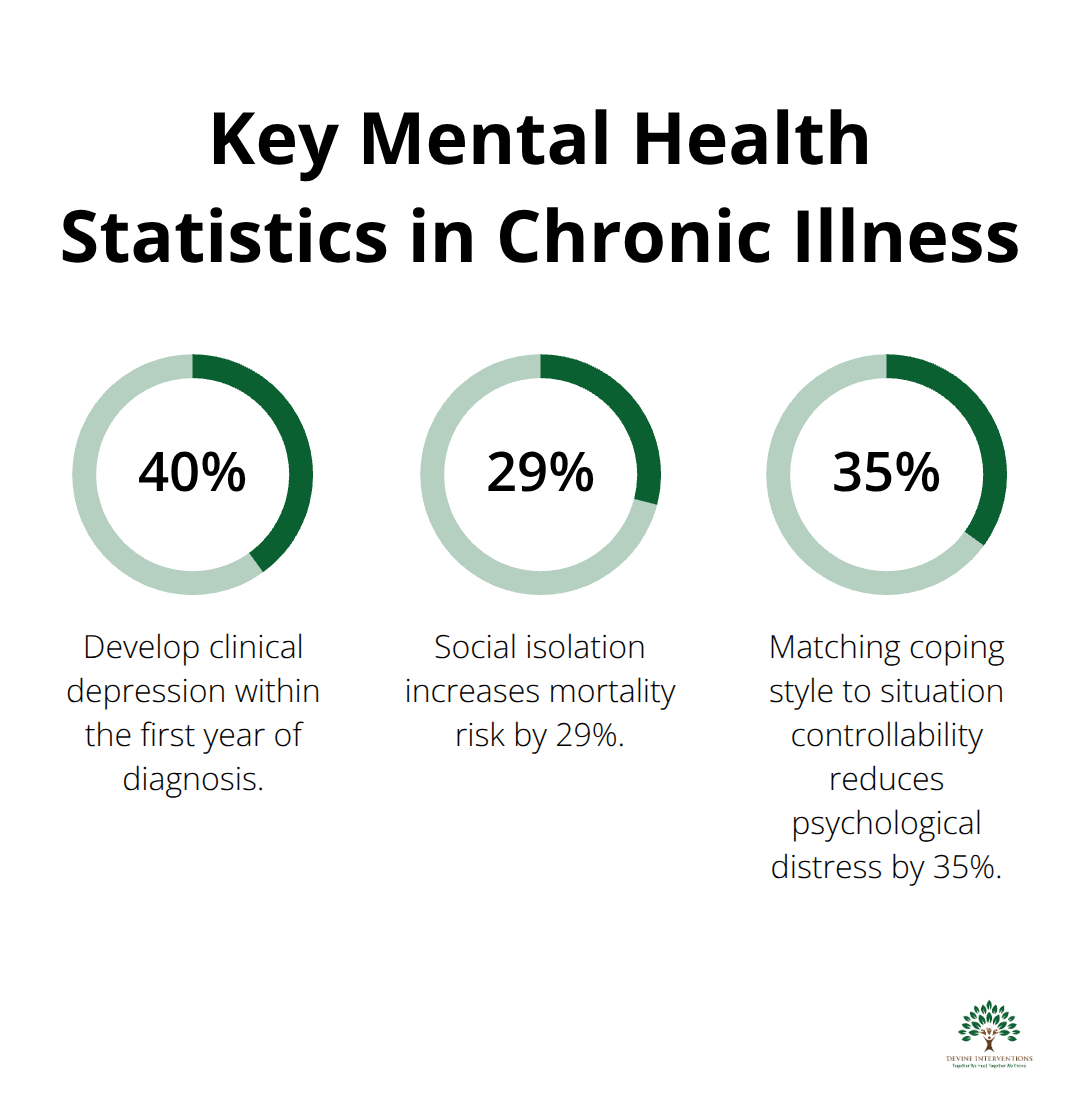
A chronic illness diagnosis triggers a predictable cascade of psychological responses that most people experience within the first six months. Research shows that approximately 40% of people with chronic conditions develop clinical depression within their first year of diagnosis. The initial shock often manifests as disbelief, followed by intense anger directed at healthcare providers, family members, or yourself.
This anger serves a protective function and temporarily shields you from the overwhelming reality of permanent health changes. Anxiety becomes your constant companion as your mind races through worst-case scenarios. You’ll likely experience what psychologists call anticipatory grief – you mourn losses that haven’t happened yet but feel inevitable. Sleep disturbances affect many newly diagnosed patients, which creates a cycle where physical symptoms worsen emotional distress.
The Reality of Daily Losses
Chronic illness forces you to grieve multiple losses simultaneously, and this grief doesn’t follow neat stages. You mourn your former identity, career aspirations, physical capabilities, and social connections all at once. The Kübler-Ross grief model, while popular, fails to capture the cyclical nature of chronic illness grief. You revisit anger, bargaining, and depression repeatedly as your condition evolves.
Financial stress compounds emotional distress. Many chronic illness patients experience significant financial hardship within two years of diagnosis. This economic pressure transforms relationships with family members who may become caregivers, financial supporters, or sources of conflict. Your spouse might struggle with increased responsibilities while you battle guilt over becoming dependent.
Social Isolation and Relationship Strain
Chronic illness exposes which relationships can withstand adversity and which cannot. Friends often disappear gradually, unable to understand your limitations or uncomfortable with your changed circumstances. Many people with chronic conditions lose a significant portion of their social circle within years of diagnosis.
This isolation isn’t just painful – it’s medically dangerous. Research demonstrates that social isolation increases mortality risk by 29%, with health consequences comparable to smoking. Family dynamics shift dramatically as everyone adjusts to new roles and expectations. Children may become caregivers prematurely, while parents struggle with watching their adult child suffer.
Marriage relationships face particular strain, with higher divorce rates among couples dealing with chronic illness. The key difference between relationships that survive and those that fail lies in communication patterns established early in the diagnosis process. These emotional challenges demand active strategies to rebuild your sense of control and purpose, including effective stress management techniques and maintaining mental wellness practices.
Building Effective Coping Mechanisms
Your coping strategy must match the specific challenge you face at any given moment. Problem-focused strategies work best when you can control aspects of your situation – you schedule medical appointments, organize medications, or adapt your living space for mobility issues. These direct actions reduce stress because they address root problems. Emotion-focused strategies become necessary when circumstances remain beyond your control – you manage pain flares, process grief over lost abilities, or deal with uncertain prognoses. Research from the Journal of Health Psychology shows that people who match their coping style to situation controllability experience 35% less psychological distress than those who use mismatched approaches.
Master Your Physical Response First
Mindfulness-based stress reduction shows significant benefits in chronic illness patients according to recent studies. Start with the 4-7-8 breathing technique three times daily – inhale for 4 counts, hold for 7, exhale for 8. This activates your parasympathetic nervous system within minutes. Progressive muscle relaxation works faster than meditation for immediate pain relief. Tense each muscle group for 5 seconds, then release completely. Your body learns to distinguish between tension and relaxation (this gives you control over physical stress management responses).
Build Non-Negotiable Daily Anchors
Successful chronic illness management depends on three non-negotiable daily anchors that remain constant regardless of symptom severity. Choose one morning routine, one midday check-in, and one evening wind-down activity. Your morning anchor might be coffee while you review your medication schedule. Your midday anchor could be a 10-minute walk or gentle stretching session. Evening anchors work best when they prepare your body for restorative sleep – dim lights, cool temperatures, and no screens for one hour before bed. Research demonstrates that consistent sleep-wake cycles provide significant benefits for chronic illness management (these anchors provide stability when everything else feels chaotic).
Match Your Energy to Your Capacity
The Spoon Theory helps you visualize energy management, but practical application requires daily assessment. Rate your energy level from 1-10 each morning and plan activities accordingly. High-energy days (7-10) allow for medical appointments, social activities, or household tasks. Medium-energy days (4-6) work best for gentle exercise, meal preparation, or phone calls.
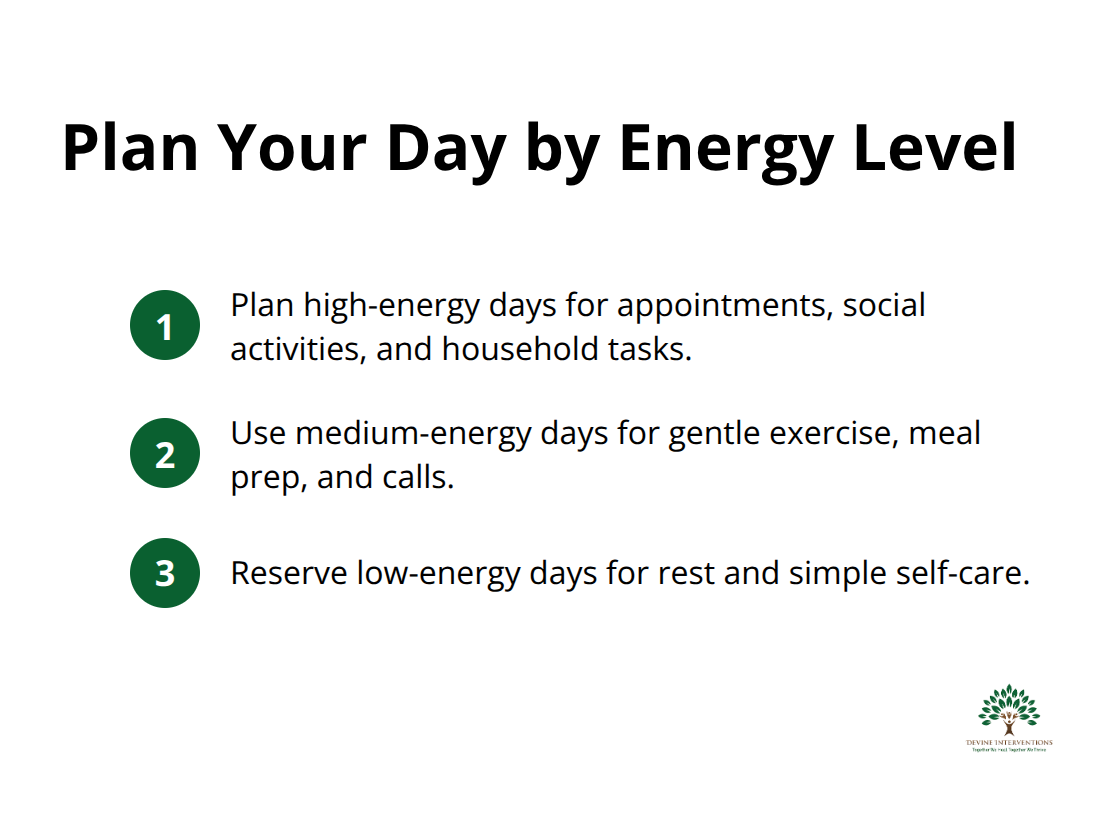
Low-energy days (1-3) demand rest, light reading, or simple self-care activities. This prevents the boom-bust cycle that worsens symptoms and creates emotional distress.
While these personal strategies form your foundation, you cannot navigate chronic illness alone. Professional support systems and community connections provide the additional resources you need to thrive rather than merely survive.
Support Systems and Professional Resources
Who Should Be on Your Support Team
Your recovery depends on the right combination of medical professionals who understand chronic illness complexity. Start with a primary care physician who coordinates all aspects of your care and maintains comprehensive medical records. This doctor becomes your advocate when specialist appointments conflict or treatments interact poorly. Add a rheumatologist, endocrinologist, or other specialists based on your specific condition, but limit specialists to three maximum to avoid fragmented care.
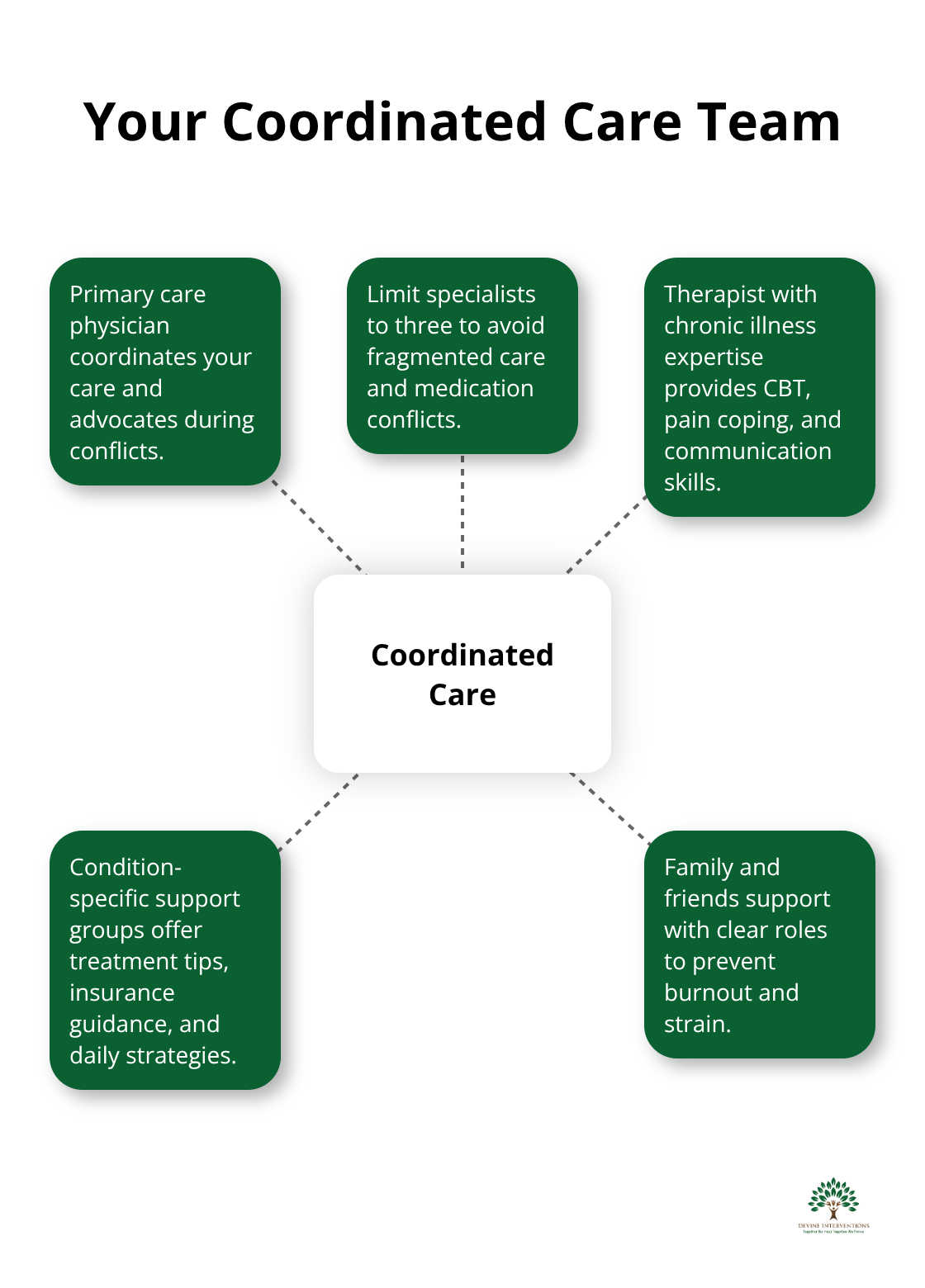
Almost half of U.S. adults have multiple chronic conditions, making coordinated care essential for preventing complications and medication interactions.
Create Your Personal Network Without Exhaustion
Family members and friends need clear boundaries about their support roles to prevent caregiver burnout and relationship damage. Assign specific tasks to different people – one person handles medical appointment transportation, another manages grocery shopping, and someone else provides emotional check-ins. This distribution prevents any single person from overwhelm. Caregivers of children with chronic illnesses often experience varying levels of burden, influenced by multiple psychosocial and environmental factors when support responsibilities aren’t distributed properly.
Join condition-specific support groups through organizations like the Arthritis Foundation or American Diabetes Association rather than generic chronic illness groups. Disease-specific groups provide practical advice about treatments, insurance navigation, and daily management strategies that generic groups cannot offer.
Professional Mental Health Support That Works
Cognitive behavioral therapy produces measurable improvements in chronic illness patients within 12-16 sessions according to multiple clinical trials. Choose therapists with specific chronic illness experience rather than general practitioners who may not understand medical trauma or anticipatory grief patterns. Therapy sessions should focus on practical coping skills, pain management techniques, and relationship communication strategies rather than endless processing of diagnosis trauma.
Schedule mental health appointments during your highest energy periods to maximize therapeutic benefit and avoid cancellations that disrupt treatment momentum. Look for providers who offer comprehensive care that addresses both your mental health needs and understands the unique challenges chronic illness presents. This integrated approach produces better outcomes than fragmented care.
Final Thoughts
Effective coping strategies for chronic illness demand consistent daily practices, professional support, and realistic expectations about your path forward. The three anchors approach provides stability when symptoms change without warning. Medical professionals who coordinate comprehensive care and mental health specialists who understand chronic illness trauma form the foundation of your support team.
Research shows that integrated treatment approaches produce better outcomes than fragmented care across multiple providers. Professional support transforms chronic illness management from daily survival into sustainable wellness practices. Your emotional wellness deserves the same attention and resources as your physical symptoms (this balance creates long-term improvement in quality of life).
We at Devine Interventions offer comprehensive mental health services that address both the psychological impact of chronic illness and practical coping skill development. Our evidence-based approach combines individual therapy, medication management, and case management services. Professional support makes the difference between managing symptoms and thriving with your condition.