Postpartum depression affects countless new mothers, yet many struggle in silence. At Devine Interventions, we understand the profound impact this condition can have on families.
Our team is dedicated to providing compassionate care and personalized support for those battling postpartum depression. We’re here to listen, understand, and guide you towards recovery with evidence-based treatments and a supportive community.
What Are the Signs of Postpartum Depression?
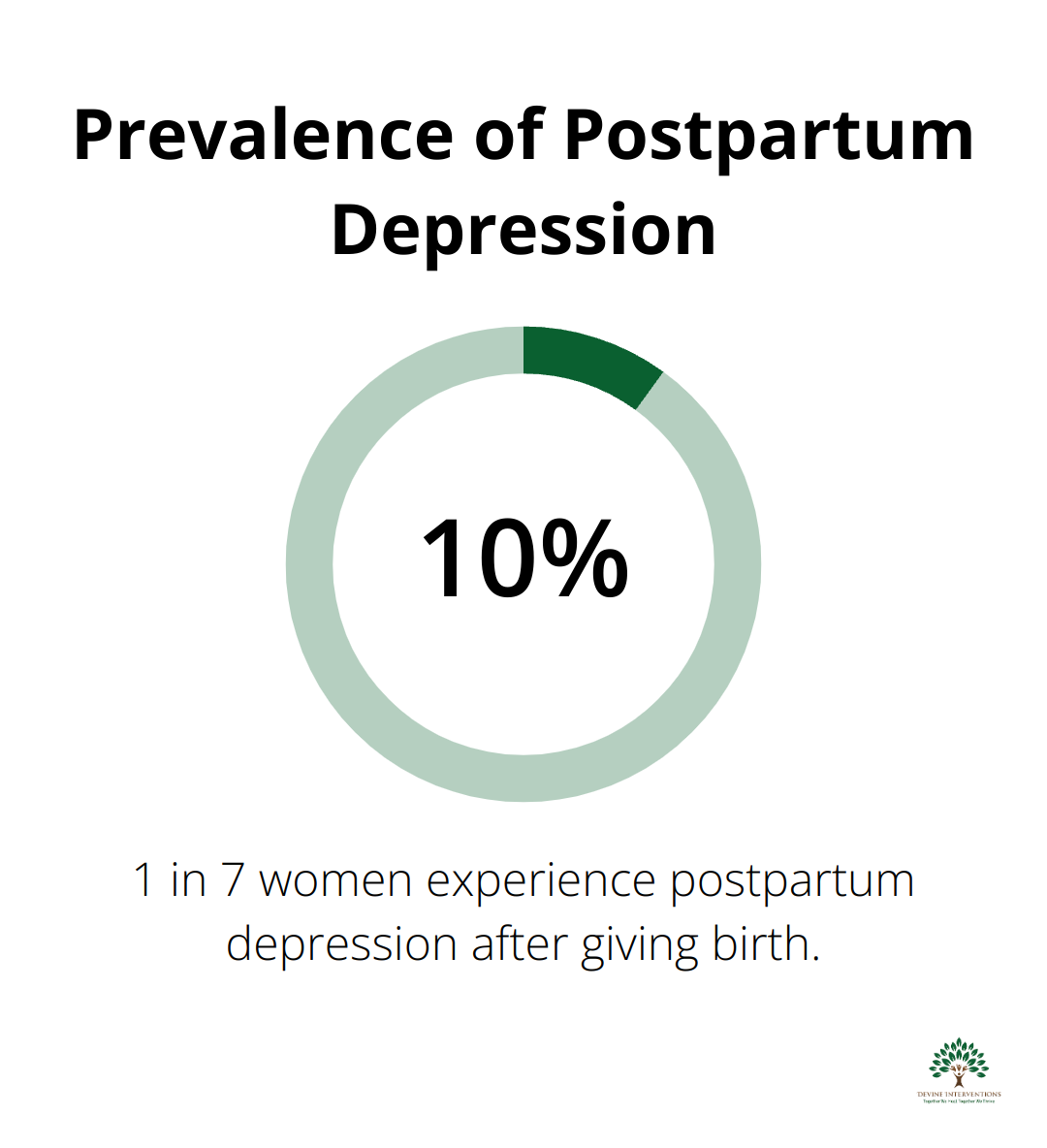
Postpartum depression (PPD) affects around 10% of women, or 1 in 7 women, after giving birth. At Devine Interventions, we’ve seen how early recognition can make a world of difference.
Recognizing the Symptoms
PPD symptoms often appear within the first few weeks after childbirth, but can start anytime during the first year. Key signs include:
- Persistent sadness or emptiness
- Severe mood swings
- Difficulty bonding with the baby
- Withdrawing from family and friends
- Changes in appetite or sleep patterns
- Overwhelming fatigue or loss of energy
- Intense irritability or anger
- Feelings of worthlessness or guilt
- Difficulty concentrating or making decisions
- Thoughts of harming yourself or the baby
If these symptoms persist for more than two weeks, it’s important to seek help. Having these feelings doesn’t make you a bad mother – it means you need support.
Debunking Common Myths
Many misconceptions surround PPD, which can prevent mothers from seeking help. Let’s clear up some common myths:
Myth: PPD is just the “baby blues” and will go away on its own.Fact: While baby blues typically resolve within two weeks, PPD is a more serious, long-lasting condition requiring professional help.
Myth: Only weak or bad mothers get PPD.Fact: PPD can affect any mother, regardless of personality, background, or parenting skills. It’s a medical condition (not a character flaw).
Myth: Admitting to PPD means you’ll lose your baby.Fact: Seeking help for PPD shows you’re a responsible parent. Treatment helps you care for your baby better, not take your baby away.
The Ripple Effect on Families
PPD doesn’t just affect mothers – it impacts the entire family. Untreated PPD can lead to:
- Difficulty bonding with the baby, potentially affecting the child’s emotional and cognitive development
- Strain on partner relationships, as partners may feel helpless or overwhelmed
- Challenges in caring for older children, who may feel neglected or confused
- Increased risk of chronic depression for the mother if left untreated
Our comprehensive approach addresses not just the mother’s symptoms, but also provides support for partners and family members. We believe in treating the whole family system to ensure the best outcomes for everyone involved.
Taking the First Step
Don’t let PPD steal the joy of motherhood. If you recognize these signs in yourself or a loved one, it’s time to take action. Our team at Devine Interventions is ready to listen, understand, and provide the compassionate care you deserve. The next step in your journey towards healing is understanding how our personalized treatment plans can help you overcome PPD and reclaim your life.
How Devine Interventions Provides Compassionate Care
At Devine Interventions, we’ve developed a unique approach to treat postpartum depression (PPD) that combines clinical expertise with genuine compassion. Our goal is to create a supportive environment where mothers and families can heal and thrive.
Personalized Treatment Plans
We recognize that every mother’s experience with PPD is unique. Our process starts with a comprehensive assessment to understand your specific situation, including your mental health history, family dynamics, and current challenges. Based on this assessment, we collaborate with you to develop a personalized treatment plan that addresses your individual needs and goals.
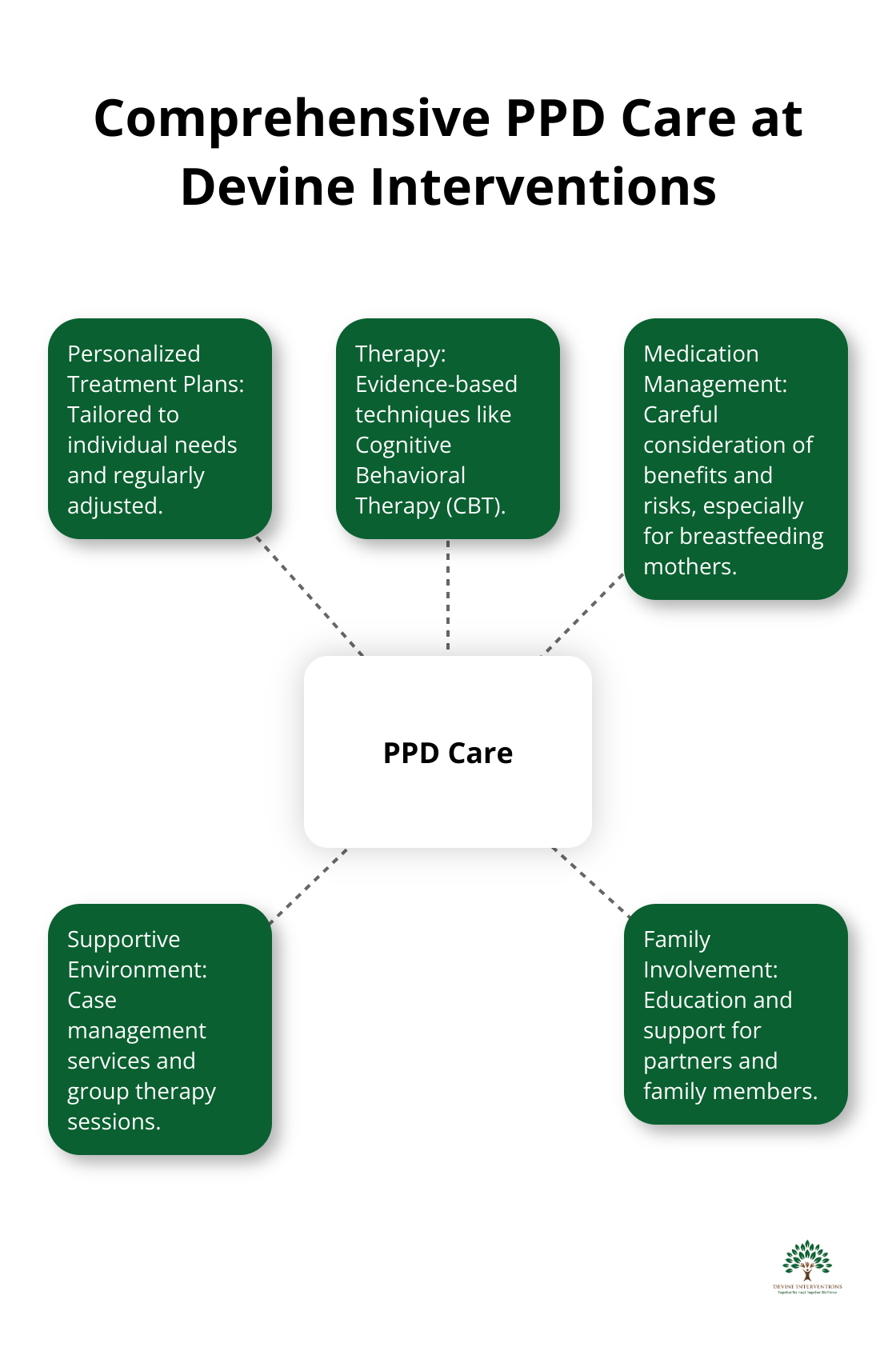
Our treatment plans are flexible and adaptable. We regularly review and adjust your plan based on your progress and changing needs. This ensures that you always receive the most effective care possible.
Therapy and Medication Management Integration
We believe in a holistic approach to treat PPD. For many mothers, a combination of therapy and medication management proves most effective. Our team of experienced therapists uses evidence-based techniques like Cognitive Behavioral Therapy (CBT) to help you develop coping strategies and build resilience.
If medication is part of your treatment plan, our psychiatric providers offer comprehensive medication management. We carefully consider the potential benefits and risks (especially for breastfeeding mothers) to find the right medication and dosage for you. When PPD is severe or there is an insufficient response to psychotherapy, antidepressant medication may be considered as part of the treatment plan.
Supportive Environment Creation
Recovery from PPD doesn’t happen in isolation. We focus on creating a supportive environment that extends beyond our office walls. Our case management services bridge clinical treatment with real-world support, helping you navigate challenges and connect with community resources.
We also offer group therapy sessions where you can connect with other mothers experiencing similar challenges. These sessions provide a safe space to share experiences, learn from others, and build a supportive network.
Family Involvement and Education
For partners and family members, we provide education and support to help them understand PPD and how to best support you. We believe that involving loved ones in the treatment process can significantly improve outcomes and strengthen family bonds.
At Devine Interventions, we commit to provide the compassionate, comprehensive care you need to overcome PPD and reclaim your joy in motherhood. Our team is here to listen, understand, and support you every step of the way. The next step in your journey is to build a strong support network that will help you through this challenging time.
How to Build a Strong Support Network
Involve Your Partner and Family
Your partner and close family members are essential to your recovery from postpartum depression (PPD). Talk openly with them about your feelings, concerns, and needs. Encourage them to learn about PPD through classes at local hospitals or community centers.
Give specific tasks to your support network. They can help with household chores, watch the baby so you can rest, or go with you to appointments. Recent research suggests that partner support during childbirth is associated with lower rates of postpartum depression, anxiety, and childbirth-related post-traumatic stress.
Connect with Other Mothers
Peer support can make a big difference. Find local PPD support groups in your area. Hospitals, community centers, and organizations often offer these groups. If you can’t attend in-person meetings, try online support groups or forums.
Talking to others who understand your experience can validate your feelings and reduce isolation. Recent studies have shown that postpartum depression affects 10%–15% of women globally, highlighting the importance of support networks.
Use Community Resources
Your community likely offers various resources to support new mothers. Here are some steps to take:
- Call your local health department or community center. They often have programs for new mothers, including home visits from nurses or social workers.
- Ask if your workplace has an Employee Assistance Program (EAP). These programs can provide counseling services and resources for managing PPD.
- Look for local parenting classes or new mom groups. These can offer both education and social connection.
- Join a mommy-and-me exercise class. Physical activity can help with PPD symptoms, and these classes let you meet other mothers.
- Find respite care services in your area. These services give you a break from caregiving and allow you time to rest and recharge.
Maintain Your Support Network
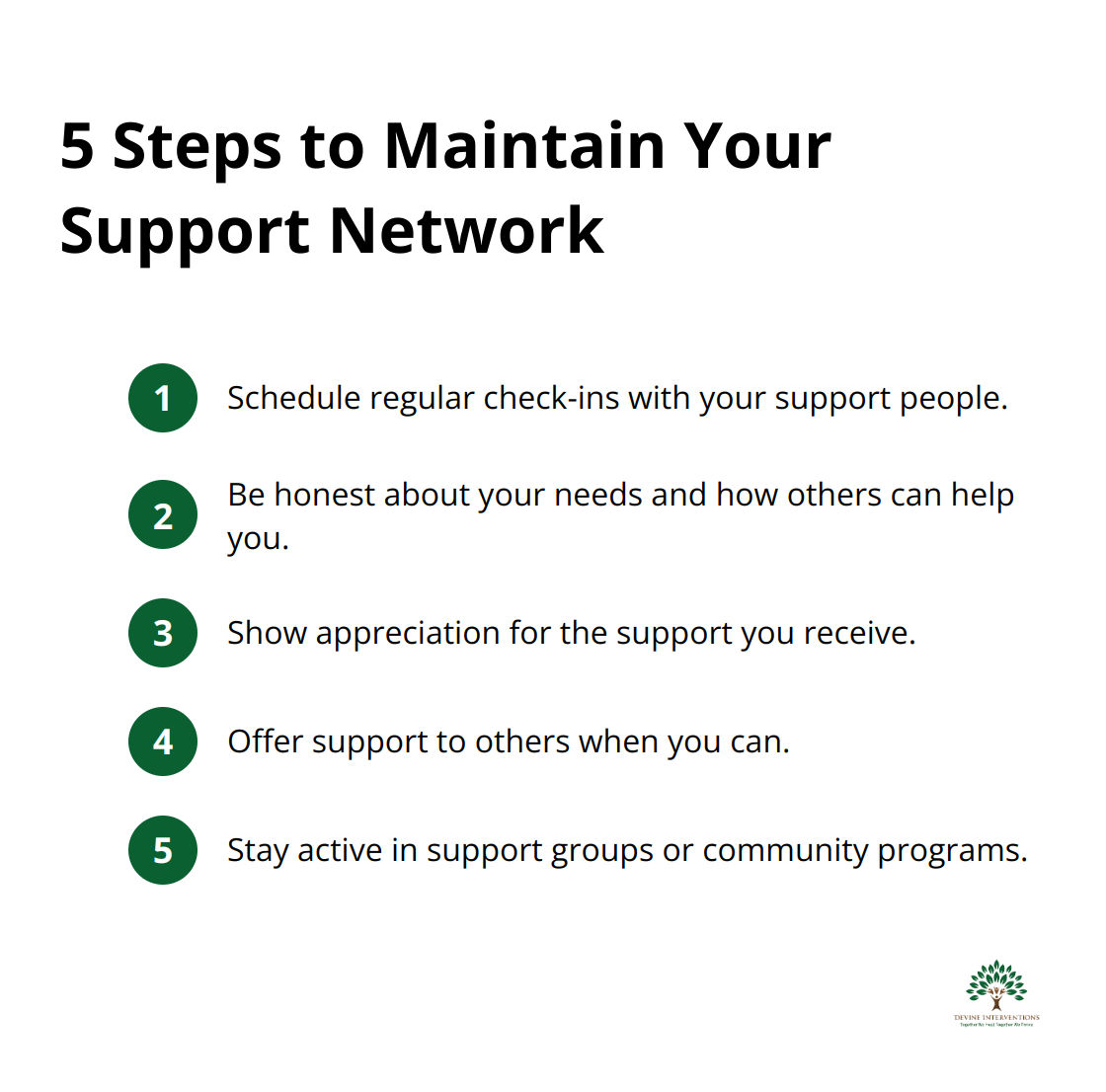
Once you’ve built your support network, it’s important to keep it strong:
- Schedule regular check-ins with your support people (even a quick text can help maintain connections).
- Be honest about your needs and how others can help you.
- Show appreciation for the support you receive (a simple “thank you” goes a long way).
- Offer support to others when you can. Supporting others can boost your own mental health.
- Stay active in support groups or community programs that have been helpful to you.
At Devine Interventions, we understand the importance of a strong support network in overcoming PPD. Our team can help you connect with local resources and support groups that complement your treatment plan. We’re here to support you every step of the way on your journey to recovery.
Final Thoughts
Postpartum depression affects many new mothers, but help and hope exist. At Devine Interventions, we offer comprehensive care to support you through this challenging time. Our approach combines personalized treatment plans, evidence-based therapies, and medication management when necessary.
We create a supportive environment that extends beyond our office, involving partners and family members in the healing process. Our team at Devine Interventions dedicates itself to help you reclaim your joy in motherhood and build a healthier future for your family. We offer a range of services, from intensive outpatient programs to individual therapy, all designed to meet your unique needs.
If you struggle with postpartum depression symptoms, we encourage you to reach out for help. Taking that first step can feel daunting, but it moves you powerfully towards healing. Your well-being matters, and we stand ready to support you every step of the way.