PTSD triggers can strike without warning, leaving you feeling overwhelmed and out of control. The sudden rush of memories, emotions, and physical sensations can be frightening and disruptive to daily life.
Learning effective coping strategies for PTSD triggers is essential for reclaiming your sense of safety and stability. We at Devine Interventions understand how challenging this journey can be, and we’re here to guide you through proven techniques that can help you manage these difficult moments and build resilience for the future.
What Actually Triggers PTSD Episodes
PTSD triggers fall into two distinct categories that affect people differently. External triggers include specific places like hospitals or parking lots, certain sounds such as sirens or fireworks, particular smells including smoke or perfume, and visual cues like crowded spaces or uniforms. Internal triggers operate from within your mind and body – racing thoughts about safety, physical sensations like rapid heartbeat or sweating, specific emotions such as helplessness or anger, and even certain body positions that remind you of the trauma.
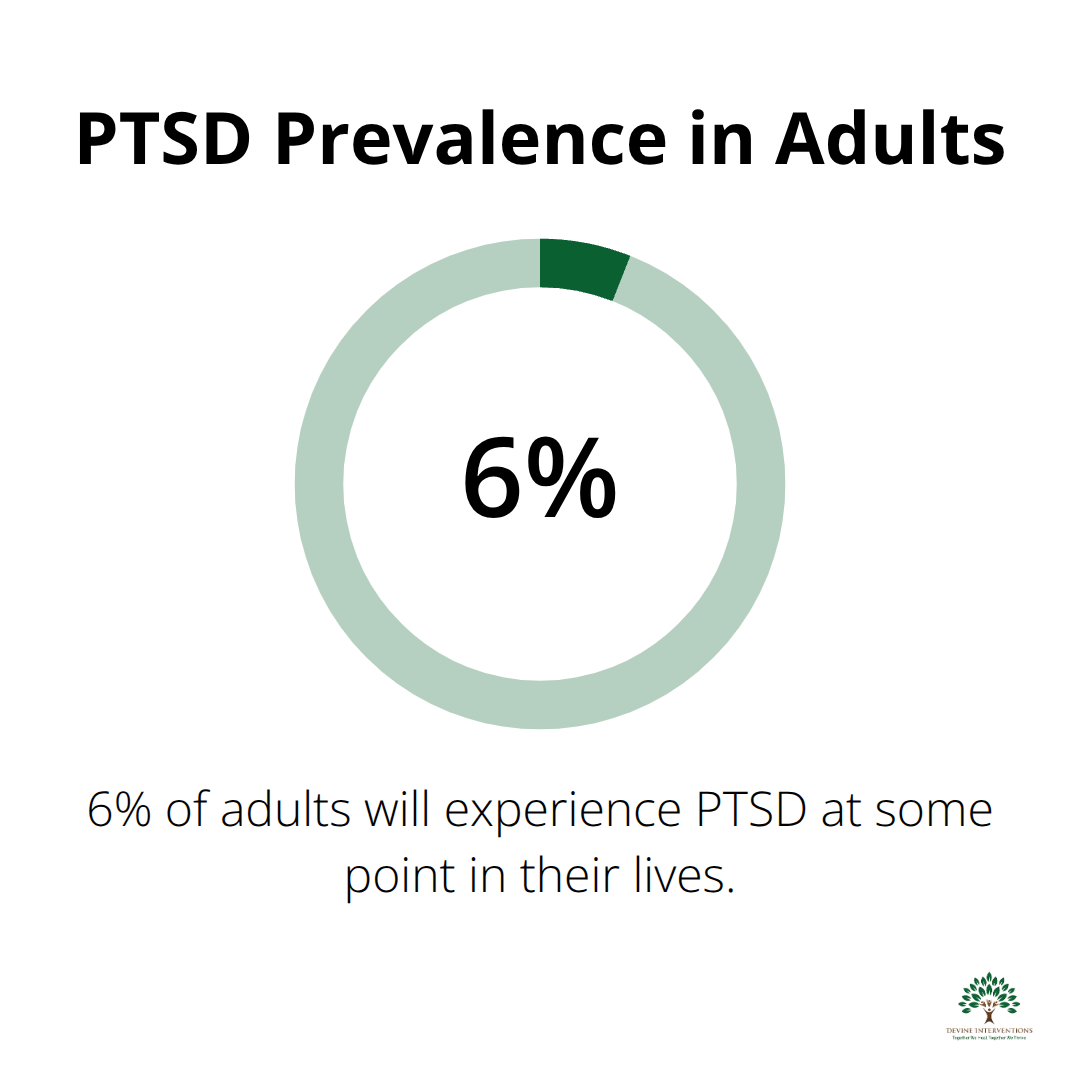
Research shows that 6% of adults will experience PTSD at some point in their lives. Your brain creates these trigger associations as it attempts to protect you, connecting present situations with past danger through learned responses.
Physical Warning Signs Your Body Sends
Your body provides clear signals when a trigger activates your PTSD response. Heart rate increases dramatically, often jumping from 70 beats per minute to over 120 within seconds. Breathing becomes shallow and rapid, muscles tense throughout your shoulders and jaw, and you may experience sudden sweating or chills.
These physical symptoms occur because your nervous system cannot distinguish between past trauma and present safety. Research indicates that physical activity can play a role in lowering mental health symptoms, making body awareness your first line of defense.
Emotional Responses That Follow Triggers
Emotional symptoms typically cascade after physical ones, creating a predictable pattern you can learn to interrupt. Intense fear arrives first, followed by feelings of helplessness, anger, or numbness. Many people describe feeling disconnected from their surroundings or experiencing time distortion where minutes feel like hours.
Concentration becomes nearly impossible, and you might feel an overwhelming urge to escape or freeze completely. Studies from trauma treatment centers indicate that emotional symptoms last an average of 20-45 minutes when left unmanaged. Co-occurring conditions such as depression and anxiety disorders often accompany these responses.
How Triggers Develop Over Time
Triggers form through your brain’s natural survival mechanism, which creates protective associations between current experiences and past trauma. Your amygdala (the brain’s alarm system) stores these connections without your conscious awareness, activating fight-or-flight responses when it detects similar patterns.
This process explains why seemingly unrelated situations can provoke intense reactions. A specific cologne might trigger memories because someone wore it during your traumatic experience, or a particular time of day might activate symptoms because that’s when the original event occurred.
The good news is that understanding these patterns gives you power to develop effective coping strategies that can significantly reduce both the intensity and duration of triggered responses.
Evidence-Based Coping Strategies for PTSD Triggers
Grounding Techniques That Stop Symptoms Fast
The 5-4-3-2-1 technique halts PTSD symptoms within 3-5 minutes when you practice it correctly. You name 5 things you can see, 4 things you can touch, 3 things you can hear, 2 things you can smell, and 1 thing you can taste. This method activates your prefrontal cortex and overrides your amygdala’s panic response. Grounding techniques help veterans lower stress levels and improve emotional regulation when used consistently.
Box breathing delivers equally powerful results. You inhale for 4 counts, hold for 4, exhale for 4, and hold for 4. You repeat this cycle 8-10 times to reset your nervous system completely. This technique works because it activates your parasympathetic nervous system (your body’s natural calm response).
Cognitive Behavioral Therapy Approaches
CBT teaches you to challenge catastrophic thoughts that fuel PTSD reactions. When triggers activate, your brain generates thoughts like “I’m in danger right now” or “This will never end.” CBT helps you replace these with accurate statements: “This feeling is temporary” and “I am safe in this moment.”
Trauma-focused therapies like CPT and PE have the strongest evidence for treating PTSD. Thought records track your automatic responses and help you identify patterns while you develop healthier alternatives. You write down the situation that triggered you, your immediate thought, the emotion it created, and a more balanced perspective.
Mindfulness and Present-Moment Awareness
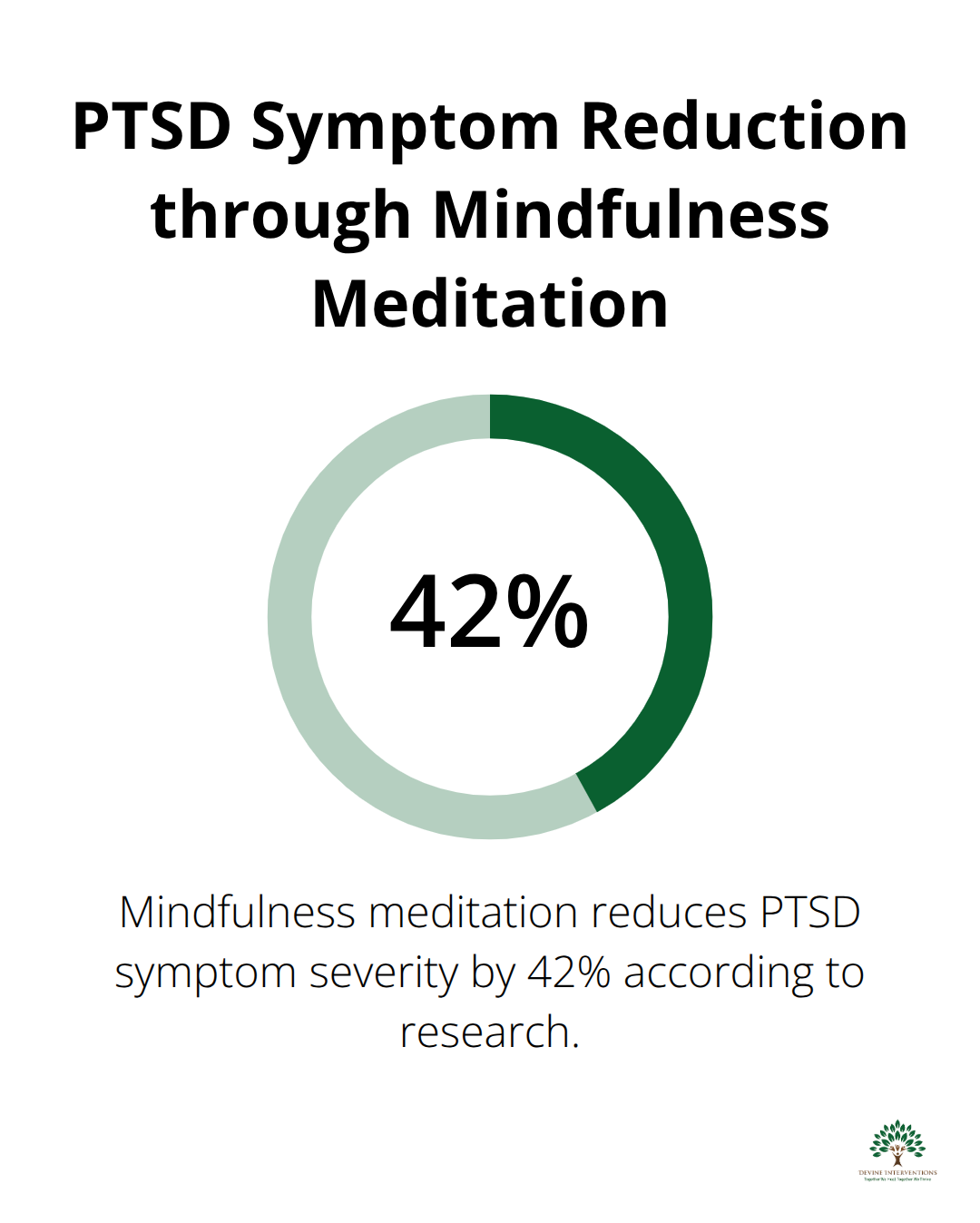
Mindfulness meditation reduces PTSD symptom severity by 42% according to research from Johns Hopkins University. The STOP technique works instantly: Stop what you’re doing, Take a breath, Observe your thoughts and feelings without judgment, then Proceed with intention.
Body scanning helps you reconnect with the present as you systematically notice sensations from your toes to your head. This practice interrupts dissociation and grounds you in current reality rather than traumatic memories. You can practice this technique anywhere, making it particularly valuable when triggers catch you off guard.
These evidence-based strategies form the foundation of effective trigger management, but they work best when combined with a comprehensive support system and personalized safety plan.
Build Support That Actually Works
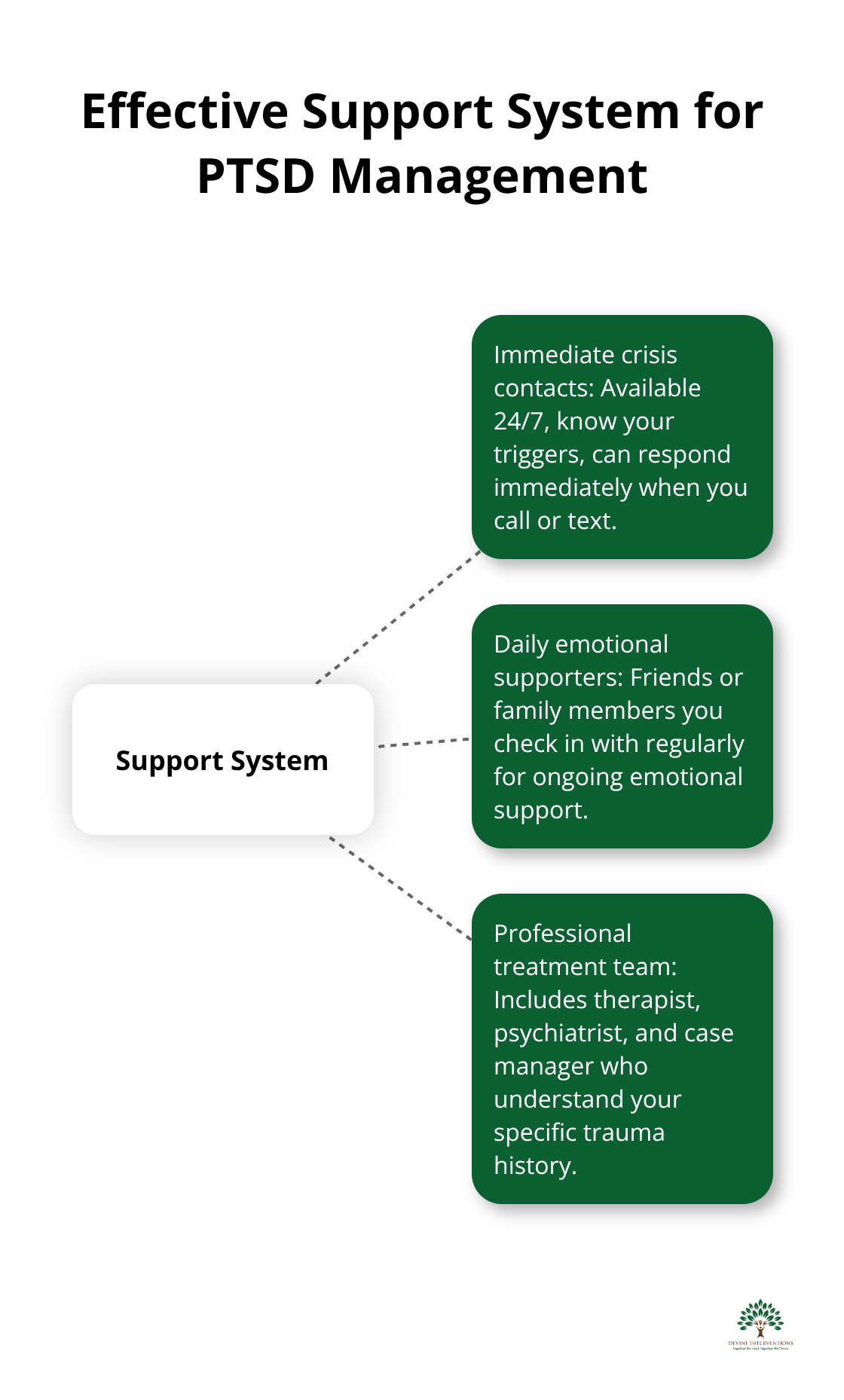
Effective support systems require three distinct categories of people: immediate crisis contacts, daily emotional supporters, and professional treatment teams. Research shows that people with strong support networks demonstrate resilience patterns, with studies indicating that most individuals (65.7%) following potentially traumatic events show resilience trajectories. Your crisis contacts must include someone available 24/7 who knows your triggers and can respond immediately when you call or text. Daily supporters are friends or family members you check in with regularly, while your professional team includes your therapist, psychiatrist, and case manager who understand your specific trauma history.
Create Your Personal Trigger Management Blueprint
Your trigger management plan must specify exact actions for before, during, and after trigger episodes occur. Write down your top five triggers and create a detailed response protocol for each one. If crowded spaces trigger you, your plan might include arriving early to events, identifying exit routes immediately, and having a code word to signal your support person that you need to leave.
Include your grounding techniques, breathing exercises, and phone numbers of three people you can call immediately. Research shows that people with written safety plans experience better treatment outcomes and improved crisis management.
Your plan should also specify warning signs that indicate you need professional intervention (such as persistent sleep disruption lasting more than five days, increased substance use, or thoughts of self-harm).
Identify Your Professional Treatment Team
Professional help becomes necessary when your coping strategies stop working consistently, when you experience thoughts of harming yourself or others, or when PTSD symptoms interfere with work or relationships for more than two weeks straight. Contact emergency services or call 988 if you have active suicidal thoughts.
Schedule an urgent appointment with a mental health professional if you notice increasing isolation, significant changes in sleep or appetite, or if family members express concern about your behavior. Narrative exposure therapy can be particularly effective for processing traumatic memories in a structured way.
Know When Crisis Intervention Is Needed
Warning signs that require immediate professional attention include persistent nightmares that prevent sleep for multiple nights, inability to leave your home for several days, or panic attacks that occur multiple times daily. These symptoms indicate your current coping strategies need professional reinforcement.
Mental health professionals can adjust your treatment plan, modify medications if needed, or recommend intensive outpatient programs that provide additional structure while you regain stability.
Final Thoughts
PTSD triggers demand a comprehensive approach that combines immediate coping techniques with long-term professional support. The grounding methods, breathing exercises, and mindfulness practices we’ve discussed provide powerful tools that interrupt triggered responses when they occur. Professional treatment remains the foundation of effective PTSD recovery through evidence-based therapies like CBT and EMDR.
Your personalized trigger management plan serves as your roadmap, but it works best when you develop it alongside qualified mental health professionals. Recovery represents an ongoing journey that requires patience with yourself and commitment to the process. The coping strategies for PTSD triggers you develop today will strengthen over time with consistent practice and professional guidance.
We at Devine Interventions understand that taking the first step toward healing can feel overwhelming. Our approach combines evidence-based practices with compassionate care (offering individual therapy and specialized treatment programs). Contact us today to begin your personalized path to recovery and reclaim control over your life.