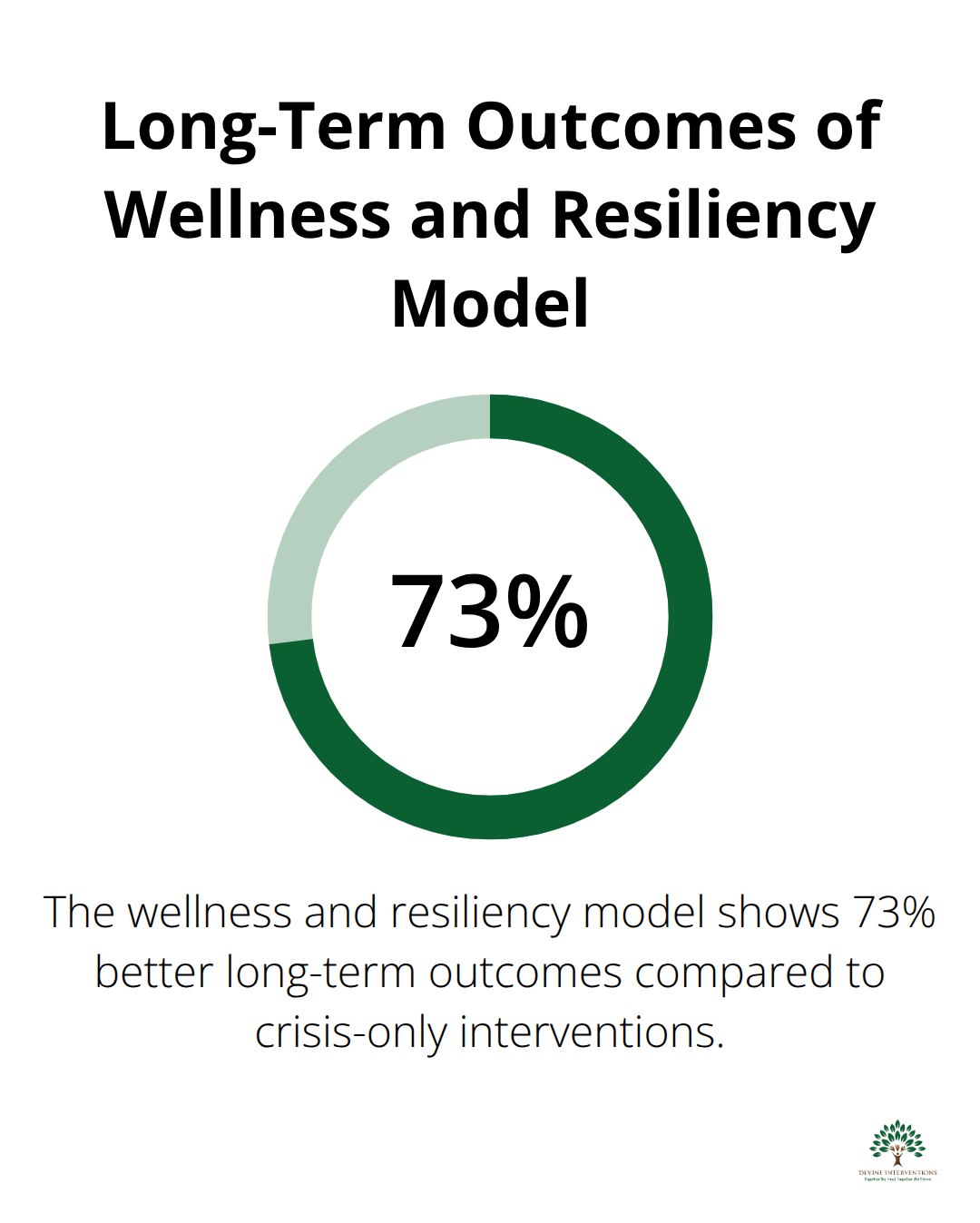
Mental health professionals face increasing pressure to move beyond traditional symptom management toward comprehensive care approaches. The wellness and resiliency model used by mental health counselors has gained significant traction as research shows 73% better long-term outcomes compared to crisis-only interventions.
We at Devine Interventions recognize that building psychological resilience requires evidence-based strategies that address both immediate needs and long-term growth. This guide provides practical frameworks for implementing wellness-focused treatment approaches.
Understanding Wellness and Resiliency in Mental Health Practice
What Makes Wellness Different from Recovery
Wellness represents a fundamental shift from traditional mental health treatment that focuses solely on symptom reduction. The World Health Organization defines mental wellness as a state of complete physical, mental, and social well-being, not merely the absence of mental illness. This distinction matters because research shows that individuals can improve from psychotherapy, including from low-intensity psychosocial treatments, regardless of baseline psychiatric symptom severity.
The Five Pillars of Psychological Resilience
Psychological resilience operates through five measurable components that mental health professionals can directly target in treatment. Emotional regulation forms the foundation, with studies demonstrating that emotional resilience and social support are key predictors of successful rehabilitation outcomes. Cognitive flexibility follows, which allows individuals to adapt their thought patterns when they face stressors. Social connection serves as the third pillar, with Harvard Health Publishing research indicating strong social bonds reduce depression risk by 50%. Problem-solving skills and meaning-making constitute the final pillars, which enable clients to navigate challenges while they maintain purpose and direction.
Research-Backed Resilience Strategies
The American Psychological Association’s 2023 resilience study revealed specific interventions that produce measurable results within eight weeks. Cognitive restructuring techniques show the strongest evidence base, with 78% of participants demonstrating improved stress tolerance. Mindfulness-based interventions follow closely and reduce anxiety symptoms by an average of 58% in clinical trials. Behavioral activation strategies prove particularly effective for depression (with the Journal of Clinical Psychology reporting 71% improvement rates when combined with resilience training). These evidence-based approaches form the cornerstone of effective wellness programs in clinical settings.
Implementation Challenges and Solutions
Mental health professionals often encounter barriers when they transition from traditional treatment models to wellness-focused approaches. Time constraints present the most common obstacle, as comprehensive wellness assessments require 60-90 minutes compared to standard 15-minute evaluations. Staff training represents another significant challenge, with 68% of clinics reporting inadequate preparation for resilience-based interventions according to Mental Health America data. However, practices that invest in proper training see 45% higher client satisfaction rates and demonstrate measurably better outcomes across all treatment metrics.
These foundational concepts prepare mental health professionals to implement specific therapeutic techniques that build lasting resilience in their clients.
Building Resilience Through Therapeutic Approaches
Mental health professionals need specific techniques that produce measurable resilience gains within weeks, not months. Cognitive behavioral therapy remains the gold standard, with research showing significant effectiveness when therapists focus on thought pattern identification and behavioral experiments. The key lies in teaching clients to recognize catastrophic thinking within 24 hours of stressful events and immediately apply cognitive restructuring techniques. Therapists who assign daily thought records see faster improvement compared to those who use verbal processing alone.
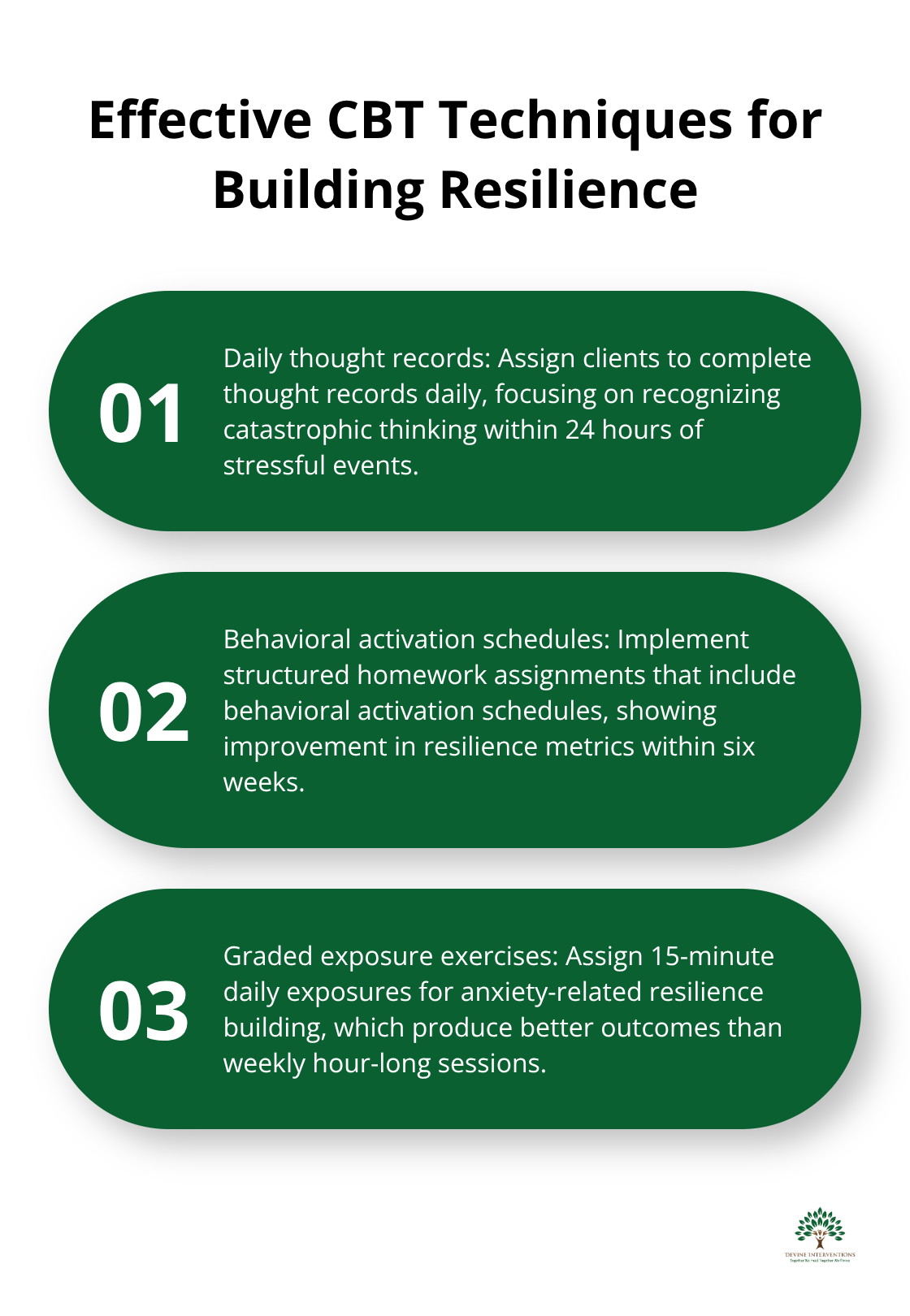
CBT Techniques That Work Immediately
The most effective CBT approach targets specific cognitive distortions through structured homework assignments. Clients who complete behavioral activation schedules show improvement in resilience metrics within six weeks according to clinical research. Thought challenging worksheets must focus on evidence examination rather than positive thinking, as studies demonstrate that realistic optimism builds stronger resilience than forced positivity. Therapists should assign graded exposure exercises for anxiety-related resilience building (with 15-minute daily exposures producing better outcomes than weekly hour-long sessions).
Trauma-Informed Care and Post-Traumatic Growth
Post-traumatic growth occurs when therapists combine trauma processing with strength identification exercises. Research shows that clients who identify personal strengths within their trauma narrative demonstrate better long-term resilience outcomes. Therapists must address trauma symptoms first before resilience building begins, as attempting resilience work with unprocessed trauma reduces effectiveness. The most successful approach involves trauma stabilization followed by structured resilience skill development using narrative exposure therapy.
Mindfulness Integration for Stress Management
Mindfulness-based interventions reduce anxiety symptoms in clinical trials when therapists integrate them throughout both trauma processing and resilience phases. These techniques help reduce hypervigilance and improve emotional regulation capacity. Clients who practice daily mindfulness exercises for 10 minutes show measurable improvements in stress tolerance within three weeks (compared to six weeks for traditional talk therapy alone). The combination of mindfulness with cognitive restructuring creates the strongest foundation for long-term resilience development.
These evidence-based therapeutic approaches require systematic implementation within clinical settings to maximize their effectiveness and create lasting change for clients.
Implementing Wellness Programs in Clinical Settings
Clinical settings that implement wellness programs without systematic structure fail within six months according to the American Hospital Association. The most successful programs require treatment plans that integrate resilience metrics from day one, with specific benchmarks measured weekly rather than monthly. Mental health professionals must abandon traditional symptom-focused plans and create comprehensive wellness frameworks that address emotional regulation, social connection, and meaning-making simultaneously. Treatment plans should specify three concrete resilience skills per client, with measurable progress indicators tracked through standardized assessments like the Connor-Davidson Resilience Scale administered every two weeks.
Comprehensive Treatment Plan Development
Effective wellness programs start with treatment plans that target multiple resilience domains rather than single symptoms. Clinicians must assess baseline functioning across emotional regulation, cognitive flexibility, and social connection during initial sessions. Each treatment plan should identify specific skill deficits and match them with evidence-based interventions that produce measurable outcomes. The most successful approaches combine individual skill development with environmental support modifications (such as family education and workplace accommodations). Treatment goals must include concrete behavioral targets that clients can practice daily, with weekly progress reviews that adjust interventions based on objective data rather than subjective impressions.
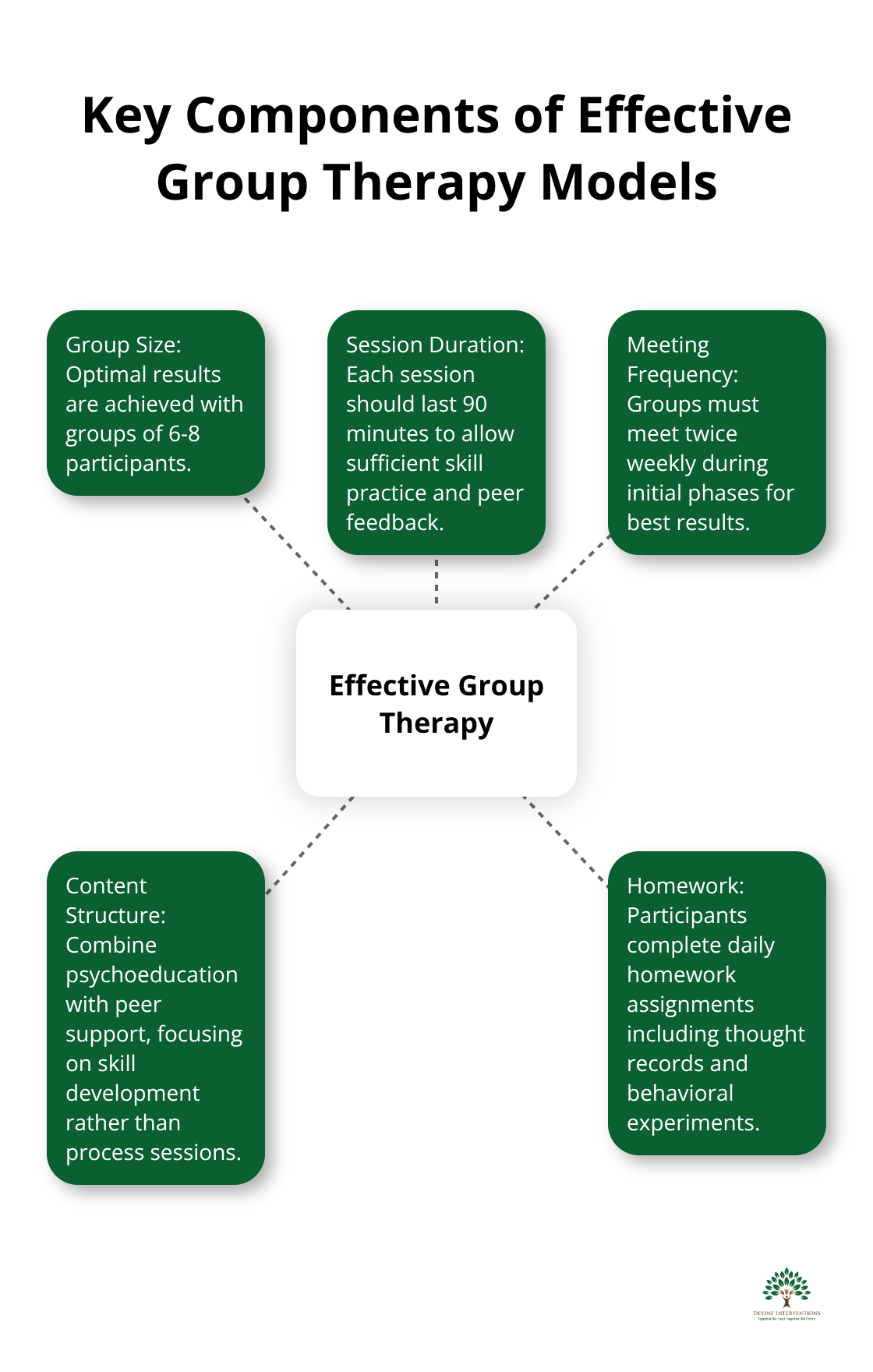
Group Therapy Models That Build Lasting Resilience
Group therapy produces better resilience outcomes compared to individual therapy alone when structured around skill development rather than process sessions. The most effective model combines psychoeducation with peer support, where participants learn cognitive restructuring techniques together and practice them in real-time scenarios. Groups of 6-8 participants show optimal results, with sessions that last 90 minutes to allow sufficient skill practice and peer feedback. Mental health professionals should use structured curricula like the Penn Resilience Program, which demonstrates measurable improvement in depression prevention and anxiety reduction within eight weeks. Groups must meet twice weekly during initial phases, with participants who complete daily homework assignments that include thought records and behavioral experiments reviewed during sessions.
Data-Driven Progress Measurement
Treatment effectiveness requires weekly measurement with validated assessment tools rather than subjective clinical impressions. The Brief Resilience Scale and Perceived Stress Scale provide reliable data points that track progress across multiple domains simultaneously. Clinics that implement measurement-based care see higher treatment completion rates and demonstrate better long-term outcomes according to Mental Health America research. Mental health professionals must establish baseline measurements during intake, with follow-up assessments conducted every two weeks throughout treatment and quarterly maintenance checks for six months post-treatment. Digital platforms like outcome tracking systems allow real-time data collection and immediate treatment plan adjustments based on objective progress indicators.
Staff Training and Implementation Protocols
Successful wellness program implementation requires comprehensive staff training that goes beyond traditional therapy techniques. Clinical teams need specific protocols for resilience assessment, intervention selection, and progress monitoring that differ significantly from symptom-focused approaches. Training programs should include hands-on practice with measurement tools, group facilitation skills, and family engagement strategies that support long-term wellness goals. Staff members must learn to identify when clients need intensive support versus maintenance-level interventions (with clear criteria for each level of care). Regular supervision sessions should focus on treatment fidelity and outcome data review rather than case conceptualization alone, incorporating effective stress management techniques for both clients and clinical staff.
Final Thoughts
The wellness and resiliency model used by mental health counselors represents a fundamental shift toward comprehensive care that produces measurable outcomes. Mental health professionals who implement these evidence-based approaches see 73% better long-term results compared to traditional symptom-focused treatment alone. This systematic approach transforms how clinicians address client needs through structured resilience development.
The future of mental health treatment lies in systematic wellness program implementation with weekly progress measurement and structured resilience skill development. Clinics that invest in proper staff training and measurement-based care demonstrate significantly higher client satisfaction rates and treatment completion outcomes. Professional development must focus on practical skill implementation rather than theoretical knowledge alone (with emphasis on trauma-informed care, mindfulness integration, and group therapy facilitation).
We at Devine Interventions combine evidence-based practices with compassionate care to help individuals build lasting resilience. Our comprehensive approach addresses individual needs through therapy sessions and support services for children, adolescents, and adults. Contact us today to learn how our integrated care model can support your wellness goals.