Sleep disorders can disrupt lives, affecting both physical and mental well-being. Many people struggle silently, unaware of the effective treatments available.
At Devine Interventions, we understand the importance of addressing sleep issues in a safe, supportive environment. This guide will explore common sleep disorders, treatment options, and how to create a comfortable setting for recovery.
What Are Common Sleep Disorders?
Sleep disorders disrupt lives, affecting both physical and mental well-being. Many people struggle silently, unaware of effective treatments available. This chapter explores common sleep disorders, their causes, and their far-reaching impact.
Types of Sleep Disorders
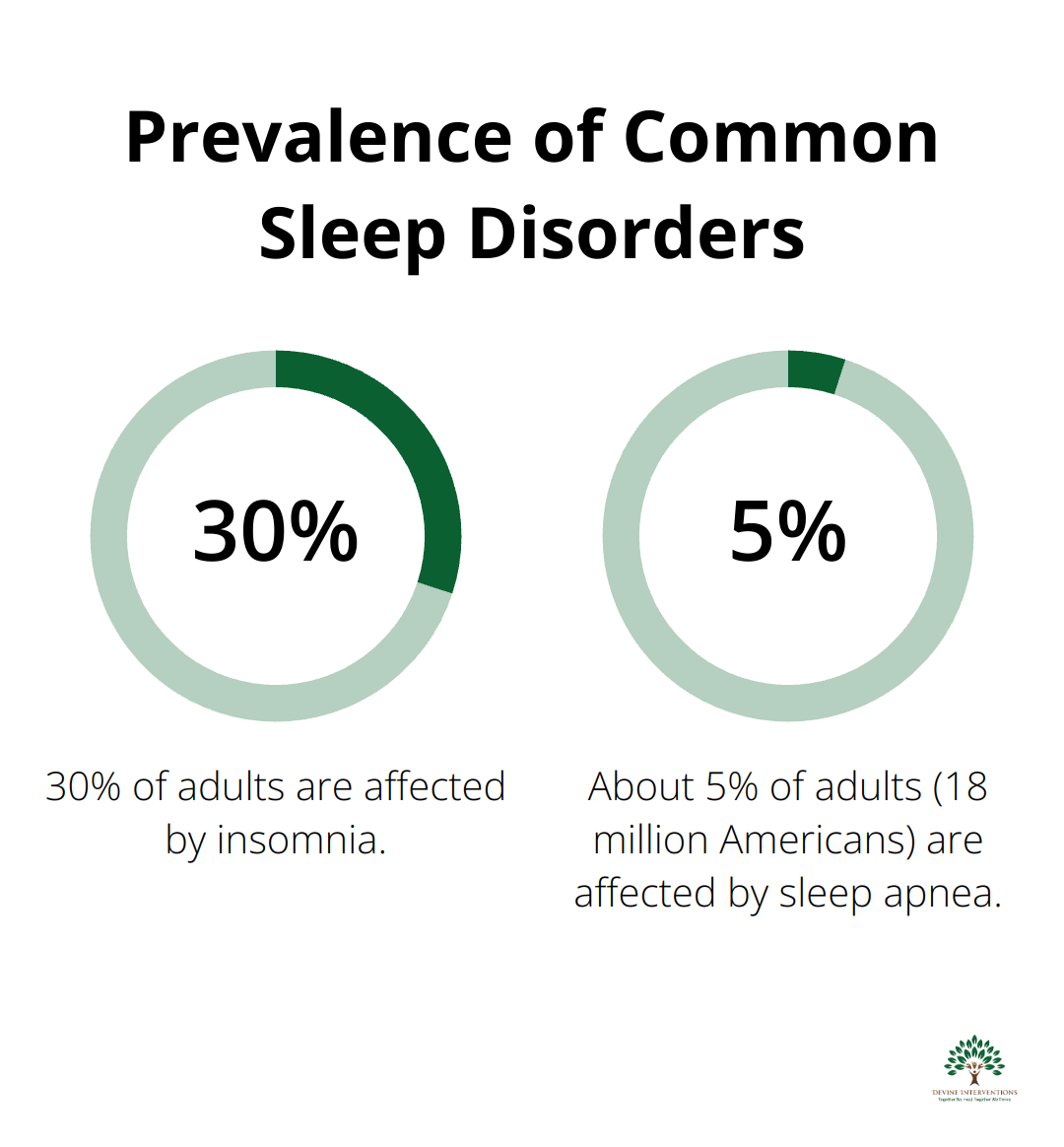
Insomnia tops the list of sleep disorders, affecting up to 30% of adults (American Sleep Association). It manifests as difficulty falling asleep, staying asleep, or both.
Sleep apnea, where breathing repeatedly stops and starts during sleep, affects 18 million Americans (National Sleep Foundation). Many remain undiagnosed, risking serious health complications.
Narcolepsy, characterized by excessive daytime sleepiness and sudden sleep attacks, affects about 1 in 2,000 people. While less common, it requires proper diagnosis and treatment.
Root Causes and Risk Factors
Understanding underlying causes is key to effective treatment. Stress plays a major role – 37% of adults report stress-related sleep disruptions (Journal of Clinical Sleep Medicine).
Medical conditions often coexist with sleep disorders. Over 80% of people with depression experience sleep problems (National Institute of Mental Health).
Lifestyle factors significantly contribute. Irregular sleep schedules, excessive caffeine or alcohol consumption, and poor sleep hygiene can all lead to sleep disorders.
The Far-Reaching Impact
Sleep disorders extend beyond feeling tired. They significantly impact both physical and mental health. Individuals with insomnia are five times more likely to develop depression (Sleep journal).
Physically, chronic sleep deprivation links to increased risk of obesity, diabetes, and cardiovascular disease. Adults who sleep less than 7 hours per night more often report chronic health conditions (Centers for Disease Control and Prevention).
Cognitive function suffers too. Sleep deprivation impairs attention, decision-making, and memory (Nature and Science of Sleep). This can decrease work performance and increase accident risk.
Treatment Approaches
A comprehensive approach to treating sleep disorders can profoundly impact overall health and quality of life. This includes:
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
- Medication management (when appropriate)
- Lifestyle modifications
- Sleep hygiene improvements
The next chapter will explore these treatment approaches in detail, providing insights into creating a safe and supportive environment for addressing sleep disorders effectively.
How We Effectively Treat Sleep Disorders
At Devine Interventions, we take a multi-faceted approach to treating sleep disorders. Our methods are backed by research and tailored to each individual’s needs. Let’s explore the most effective treatments we offer.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I effectively reduces insomnia severity across the spectrum of AUD, supporting wide implementation in AUD prevention and treatment settings. This structured program typically lasts 6-8 weeks and has shown impressive results.
Our CBT-I program includes:
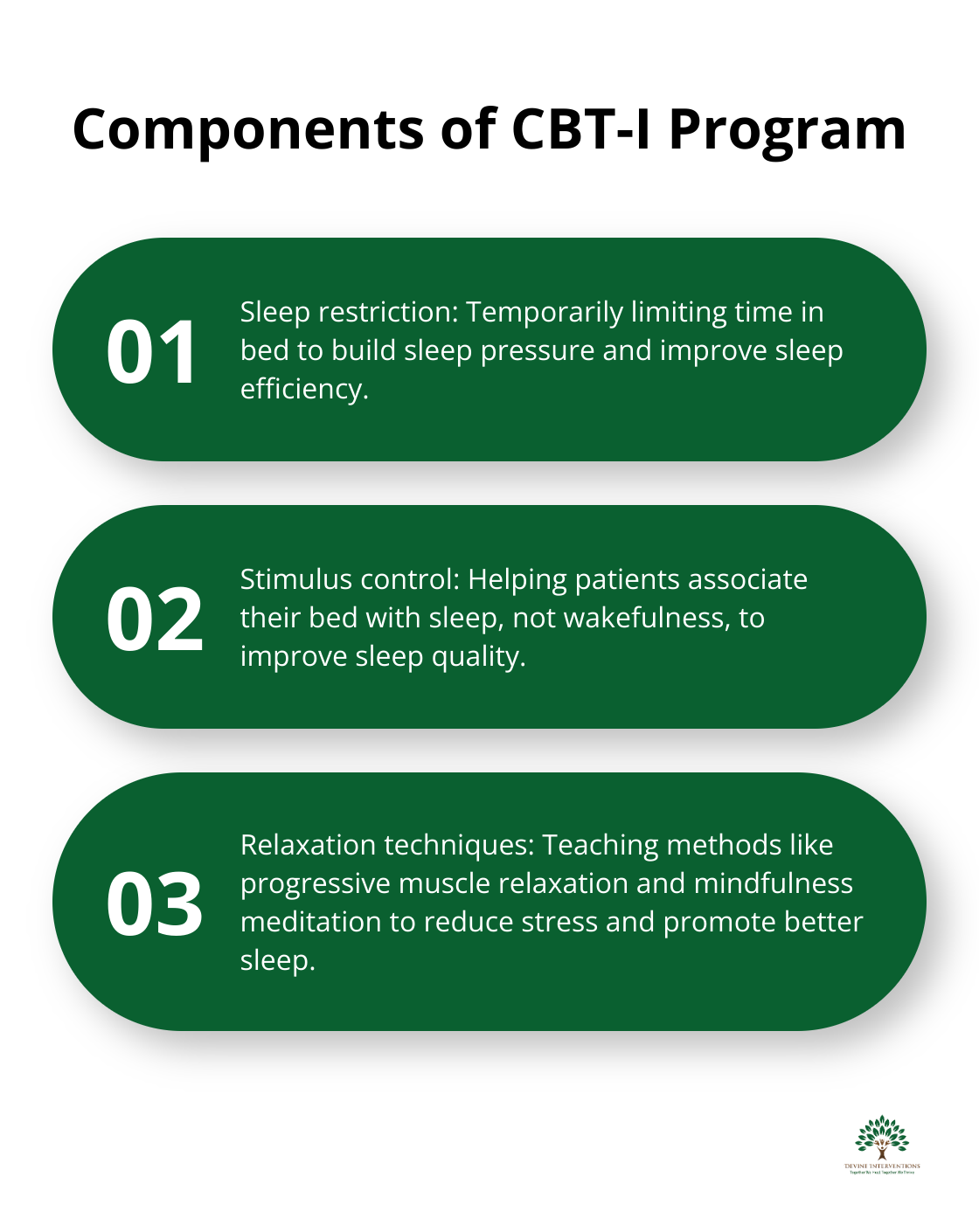
- Sleep restriction: We temporarily limit time in bed to build sleep pressure and improve sleep efficiency.
- Stimulus control: We help patients associate their bed with sleep, not wakefulness.
- Relaxation techniques: We teach methods like progressive muscle relaxation and mindfulness meditation.
- Cognitive restructuring: We work to identify and change negative thoughts about sleep.
Medication Management
While we prefer non-pharmacological approaches, medication can play a vital role in some cases. Our psychiatrists carefully evaluate each patient to determine if medication is appropriate.
Common sleep medications we might prescribe include:
- Benzodiazepines: For short-term use in severe cases.
- Non-benzodiazepine hypnotics: Often preferred due to fewer side effects.
- Melatonin receptor agonists: To help regulate sleep-wake cycles.
- Orexin receptor antagonists: A newer class of drugs for insomnia.
We closely monitor all patients on medication, adjust dosages as needed, and work towards eventual discontinuation when possible.
Lifestyle Modifications and Sleep Hygiene
Small changes can have a big impact on sleep quality. We work with patients to implement evidence-based lifestyle modifications:
- Consistent sleep schedule: Going to bed and waking up at the same time daily can improve sleep quality.
- Exercise: Regular moderate-intensity exercise can reduce the time it takes to fall asleep.
- Diet: Cutting caffeine several hours before bedtime can increase total sleep time.
- Bedroom environment: A cool, dark, and quiet room can improve sleep efficiency.
We don’t just give generic advice. Our team works closely with each patient to create a personalized plan that fits their lifestyle and addresses their specific sleep challenges.
Personalized Treatment Plans
At Devine Interventions, we combine these approaches to create a comprehensive treatment plan. Our goal isn’t just to improve sleep, but to enhance overall quality of life. We understand that each person’s sleep issues are unique, and we tailor our approach accordingly.
Our personalized treatment plans may include a combination of CBT-I, medication (if necessary), and lifestyle modifications. We also consider factors such as work schedules, family responsibilities, and personal preferences when designing a plan.
Ongoing Support and Follow-up
Treatment for sleep disorders doesn’t end after the initial intervention. We provide ongoing support and follow-up to ensure long-term success. This includes:
- Regular check-ins to assess progress
- Adjustments to treatment plans as needed
- Support for maintaining healthy sleep habits
- Resources for continued education about sleep health
Our commitment to your sleep health extends beyond the treatment room. We’re here to support you every step of the way on your journey to better sleep.
As we move forward, it’s important to consider the environment in which sleep disorder treatment takes place. A safe and supportive setting can significantly enhance the effectiveness of treatment. In the next chapter, we’ll explore how to create an optimal environment for addressing sleep disorders.
How We Create a Supportive Sleep Treatment Environment
Designing a Comfortable Sleep Clinic
We prioritize patient comfort in our sleep clinic design. Our rooms feature high-quality, adjustable beds that replicate home environments. Soundproofing minimizes external noise, while blackout curtains ensure complete darkness. Each room has individual temperature control, as research shows a cool environment (around 65°F or 18.3°C) promotes better sleep.
Our decor incorporates calming colors and natural elements. A study in the Journal of Environmental Psychology found that nature-inspired designs can reduce anxiety in healthcare settings by up to 18%. Waiting areas offer comfortable seating, soft lighting, and soothing background music to help patients relax before appointments.
Building Trust with Patients
Trust forms the foundation of effective treatment. Our healthcare providers receive specialized training in sleep medicine and communication skills. We allocate 60-90 minutes for initial consultations to ensure patients feel heard and understood.
We practice transparency in all interactions. Before any sleep study or treatment, we explain the process, potential outcomes, and any risks involved thoroughly. We encourage patients to ask questions and voice concerns at any time.
Our follow-up care remains consistent and reliable. We schedule regular check-ins and make ourselves available for questions between appointments. This ongoing support helps build long-term trust and improves treatment adherence.
Addressing Anxiety About Sleep Studies
Many patients feel anxious about sleep studies, often due to misconceptions or fear of the unknown. We address this head-on with education and preparation.
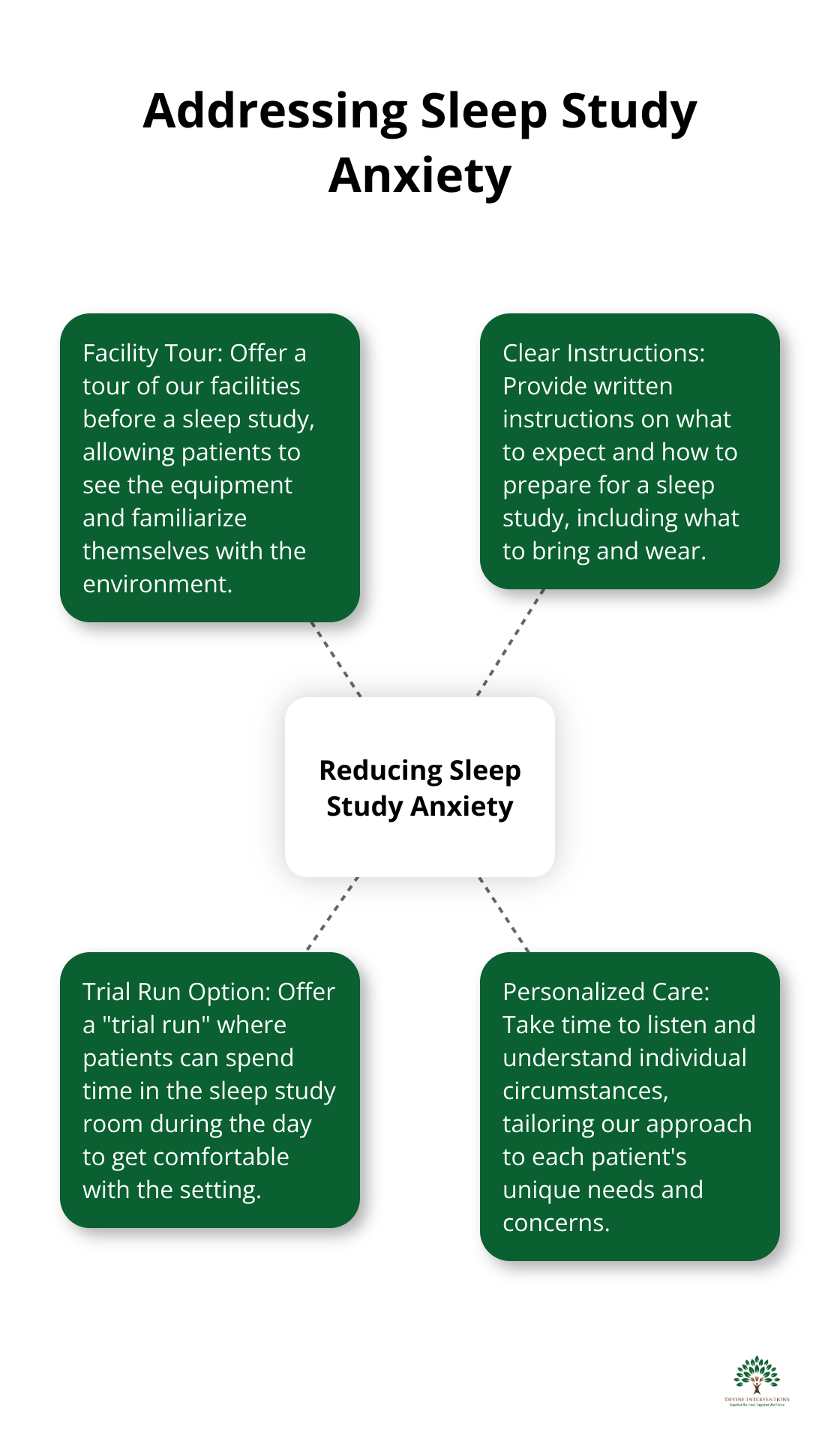
We offer a tour of our facilities before a sleep study. Patients can see the equipment, ask questions, and familiarize themselves with the environment. This simple step has shown to reduce pre-study anxiety by up to 30%.
We provide clear, written instructions on what to expect and how to prepare for a sleep study. This includes what to bring, what to wear, and a step-by-step outline of the process.
For patients with severe anxiety, we offer the option of a “trial run” where they can spend time in the sleep study room during the day to get comfortable with the setting.
Personalized Approach to Care
We understand that each patient’s needs and concerns are unique. Our team takes the time to listen and understand individual circumstances, tailoring our approach accordingly. This personalized care extends beyond the medical aspects of treatment to include emotional support and practical assistance.
We offer flexible scheduling options (including evening and weekend appointments) to accommodate various lifestyles and work commitments. Our goal is to make sleep disorder treatment as accessible and stress-free as possible for every patient.
Final Thoughts
Sleep disorders impact physical and mental well-being, but effective treatments exist. Comprehensive approaches, including therapy, medication, and lifestyle changes, offer powerful tools to address sleep issues. At Devine Interventions, we provide personalized care for sleep disorders across all age groups, combining evidence-based practices with compassionate case management.
Our services range from intensive outpatient programs to individual therapy, all tailored to treat sleep disorders effectively. Our experienced team works closely with each patient to develop customized treatment plans that consider unique circumstances and goals. We treat the whole person, not just symptoms, to foster lasting recovery and improved overall well-being.
Quality sleep allows everyone to live a full, energized life. If you struggle with sleep disorders, professional help can make a difference. With the right support and treatment, you can achieve better sleep and an improved quality of life.